Fighting Back Against Fibro Neglect
Treatment & Research News
Fighting Back Against Fibro Neglect
– See What AFSA is Doing
Home | Treatment & Research News

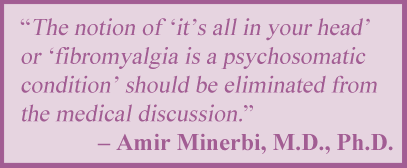
Many physicians’ websites list fibromyalgia as a condition they do not treat, and the trend is growing. These sites are dismissive of us, claiming we do not fall into their medical specialty. How convenient, since no one knows what causes fibro, let alone who should be treating it.
AFSA is pushing back against this discriminatory practice by funding research that favorably impacts your care. We initiated six studies in the past two years and one project just concluded (the impressive data will soon be published). And this is just the beginning; AFSA hopes to fund three more studies next year.
As you read through the project highlights below, we hope you feel more optimistic about your future. Our vision is that someday soon, all doctors will happily diagnose and treat this disease. Please join AFSA’s quest to identify blood markers for diagnosing fibromyalgia and develop treatments that work. It’s the only way to fight the neglect of people with fibromyalgia.
Novel Fibro Treatment

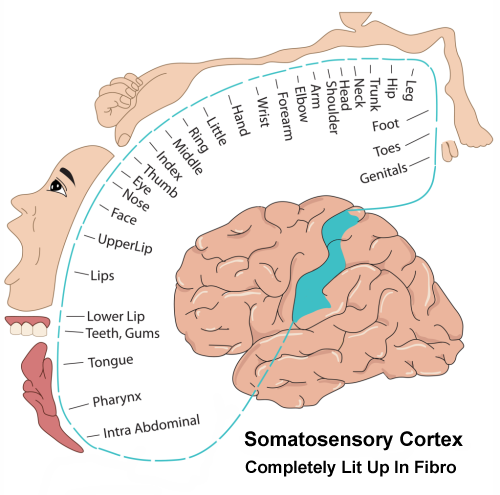
If only you could tune your brain to work the way it should. That’s the goal of this study using transcranial magnetic stimulation (TMS). The protocol packs the power of a 30-minute session into 3 minutes so the entire treatment only takes four days. The technique is used successfully to treat other conditions but this will be the first time it is used for fibromyalgia.
The trial is expected to show TMS is an effective way of improving the fibromyalgia symptoms of pain, cognitive issues, and fatigue. It will also determine how TMS works in patients by measuring changes in the brain, spinal cord, and immune system function. More details
Is Your Brain Barrier Impaired?

Immune reactive proteins in your blood (called cytokines) can impair the integrity of your blood-brain barrier (BBB). This study examines the role of cytokines and a porous BBB in producing your symptoms of pain, sleep disturbances, and fatigue. If a leaky BBB is confirmed, it offers proof that substances in the blood are disrupting brain function and that fibromyalgia is a serious disease.
Another study goal is to identify the cytokines related to key fibromyalgia symptoms. This can advance patient care in two ways. First, it becomes the starting point for identifying blood biomarkers. And second, it paves the way for developing new treatments that block specific cytokines, such as those used for inflammatory diseases. More details
What Causes Symptom Flares?

Do the malfunctions in your brain or the disruptions in your immune system drive your fibromyalgia flare episodes?1 Answering this question brings us closer to identifying the underlying cause of this disease, which is the project goal.
The brain-immune system dynamics will be measured before, during and after a major symptom flareup. This study is like looking at a video (not just a snapshot) of the processes as they unfold and the research team suspects elements of the immune system will play a flare-triggering role. If so, this will lead to therapies targeting the immune system as well as potential biomarkers for disease severity. More details
Predicting Who Benefits from Cannabis

Cannabis can relieve pain and enhance sleep, but the response varies.2 Roughly 25 percent of fibromyalgia patients are believed to reap substantial benefits while others only experience side effects. This randomized controlled trial involving 150 patients will estimate the efficacy of cannabis oil in fibromyalgia, and much more.
The gut bacteria (or microbiota) are significantly altered in fibromyalgia patients and can influence the response to medications. So, each patient’s symptoms along with the composition of their microbiota will be used to develop a prediction tool to identify who is most likely to benefit from the drug. In addition, measuring the microbiota before and after the three-month trial will determine if gut microbes change with symptom improvements. This could lay the groundwork for targeted microbiota therapy. More details
Neutrophils as a Biomarker

Neutrophils are your immune system’s front-line defense against pathogens. Preliminary evidence shows they behave differently in fibromyalgia because they are in an activated state and appear to be sensitizing neurons to cause pain.3
This study explores how the neutrophils are altered in patients and will correlate this with key fibromyalgia symptoms. It also examines the proteins they use to signal other cells in the immune system and the nearby neurons. These proteins can provide insight into disease mechanisms and, hopefully, serve as a fibromyalgia signature or biomarker. More details
Promising Treatment Trial Results
Cranial electrical stimulation (CES) uses a hand-held device to emit a pulsating current through clips attached to the earlobes. It’s FDA-cleared for treating insomnia and is believed to work by improving brain function. But can this device relieve fibromyalgia pain, fatigue, and sleep disruption?
This trial’s preliminary data shows CES reduces fibromyalgia pain and leads to favorable changes in the brain. Once all the results are officially published, we will report on them in the Projects Funded section of the website. The next step will be to get insurance companies to cover the cost of the device ($840). More details
We Are Just Getting Started …
Want to launch more projects like those above? We do too but need your help to fight back against decades of fibromyalgia neglect. We are a group of patients and family members volunteering our time. Please consider donating to AFSA (whatever you can afford) so that we can continue to fund patient relevant projects. More than 90 percent of your donation dollars go to research. We have a Four-Star rating with Charity Navigator and a Platinum Seal from Guidestar/Candid to help you give with confidence.
Don’t Miss a Beat on New Treatments & Research: Sign up for a Free Membership today.
References for Fighting Fibro Neglect
- Gomez-Arguelles JM, et al. Reumatologia 60(4):242-246, 2022. Free Report
- Boehnke KF, et al. Anesth Analg 138(1):5-15, 2024. Free Article
- Caxaria S, Sikandar S, et al. PNAS 120(17):e2211631120, 2023. Free Report