Treatment & Research News
Fibromyalgia Update on
Doctors, Treatments & Research
Home | Treatment & Research News
Developing fibromyalgia is like getting buckled into the seat of a never-ending roller coaster ride. There is no off ramp or way out. All you can hope for are compassionate doctors, effective treatments and research advances that make the ride smoother. No one questions the high prevalence of fibromyalgia, but what about your daily hassles? Here’s an update on important fibromyalgia issues and research progress that impacts your care.
Healthcare for Fibro
Most medical conditions pertain to a single organ or system in the body. This is not the case for fibromyalgia. Your symptoms involve multiple systems.
The diverse nature of fibro makes finding a good doctor essential, but who should you see? Rheumatologists developed the diagnostic criteria, yet a recent survey reveals that 90 percent don’t want fibromyalgia patients.1 Perhaps a primary care physician is more suited. After all, these “generalists” are supposed to be trained to treat the whole body. However, the survey indicates only 38 percent of primary care doctors know how to diagnose fibromyalgia, much less treat it.
If you suspect that most doctors don’t want to treat fibromyalgia, this recent report confirms your suspicions. It’s a compilation of 20 different surveys and involves nine thousand physicians, so the findings are highly significant.
So, why are you being tossed between doctor’s offices like a human volleyball? The answer has to do with perceptions. Half of physicians believe fibromyalgia is a psychosocial condition, not a real disease.
Another survey of physician attitudes reveals that fibromyalgia carries a terrible stigma in the medical community.2 Doctors confessed that if diagnosed with fibro, they would not disclose it to their colleagues. And in general, physicians said that treating your condition was not satisfying. Many providers claimed patients exaggerated their symptoms and others secretively hoped patients did not return.
Treatment Options
You know better than anyone – the treatments for fibromyalgia are disappointing. The number one endorsed therapy is exercise, which has downsides because overdoing it causes serious flare ups. Besides, research shows exercise does not phase the root cause of your fibromyalgia discomfort: reduced pain thresholds.3
Dare ask what the medical community and researchers promote as the second-best therapy for fibromyalgia? It’s cognitive behavioral therapy (CBT) or simply stated: learn to cope with your illness. Yet no surprise to you, a review of studies shows CBT provides only a six percent improvement in fibromyalgia symptoms.4 It helps you cope, but the physical benefits are imperceptible.
With regards to medications, you’ve no doubt already encountered their shortcomings. The three FDA-approved medications help one out of 7-10 fibromyalgia patients. And when it comes to alternative therapies, you are on your own to find help.
Research Offers Hope

Your physician and treatment dilemmas can be resolved if researchers identify the cause of your pain and develop biomarkers. Within the past five years, three findings possess a “wow” factor in fibromyalgia research and here’s a brief update:
- A marker that maps the widespread pain of fibro and documents inflammation throughout your brain.5 In fact, it tosses aside the old notion that your pain can be effectively treated with drugs that target neurons. Instead, the more likely target is the immune cells in your brain called microglia.
- Transferring blood from fibromyalgia patients to mice dramatically reduces the animal’s pain threshold.6 Fatigue and reduced grip strength also occurred in the mice. Something in your blood contributes to fibro and may lead the way to a diagnostic marker. Perhaps equally important, no one dares to suggest that these rodents need CBT or more exercise!
- Transferring gut bacteria from fibro patients to the intestines of mice also reduces the animal’s pain threshold.7 It even triggers the whole enchilada of metabolic and immunological findings from prior studies in patients. And another fascinating finding: depression occurred in the mice four months later (about ten human years). This clearly proves depression is not the cause of your disease.
The significance of the above discoveries is not lost on AFSA. Earlier this year, we funded three projects to build on the above findings:
- CES – evaluates the ability of this nondrug therapy to improve sleep, reduce fatigue, and decrease neuroinflammation
- Gut bacteria and Cannabis Trial – looks at the longitudinal changes in gut microbes with symptoms as well as the effectiveness of cannabis to treat fibro
- Brain-immune Interactions – assesses how immune markers in the blood affect brain function and fibro symptoms
AFSA has already solicited researchers worldwide and hopes to fund more patient-relevant projects in 2025.
The Real World
AFSA is laser-focused on funding projects with the greatest odds of impacting your care in the near future. However, we are not a large funding institution like the National Institutes of Health (NIH). We rely on donations while the NIH has a steady stream of tax dollars to fill their coffers. In 2023, the NIH claims they awarded $15 million towards fibromyalgia research.8 That’s impressive until you look at what they did with the money.
A breakdown of funds allocated by NIH shows one-fourth was diverted to study other conditions (see table). Another fourth went to fund more exercise and behavioral studies. Eight percent went to rodent models that had absolutely nothing to do with fibromyalgia.
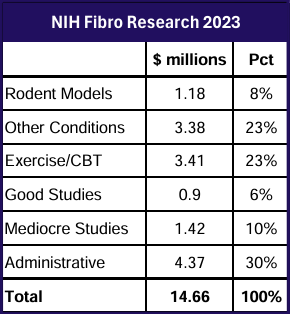
Out of the 31 studies funded under the guise of fibromyalgia research, only three are good projects. One is a biomarker study. Another tests an old drug that shows promise. And the third project examines brain function in children initially developing fibromyalgia.
Hoping to see more exciting studies funded by your tax dollars? You generally won’t find a wow factor in NIH projects. Instead, they tend to reward the same researchers over and over again with their baby step approaches. While you are eager to see progress, scientists don’t have the same motivation. In addition, every researcher’s institution skims 30 percent off the top from each award for administrative services.
There’s another facet of the NIH process you should be aware of. The higher-ups making the funding decisions are like the physicians who do not want to treat you. That’s why so much of the budget for fibromyalgia is diverted to other diseases, like arthritis and lupus. Even at NIH, there’s a stigma surrounding your illness. The assumption that you just need to cope and exercise regularly still prevails.
You Deserve More
Whether you are work-disabled or hold a job, life is a constant struggle. Lack of physician empathy and ineffective treatments compound your burden of living with fibromyalgia.
Your greatest chance for a better life hinges on research, but not just any research. It must be innovative and focused on areas that improve your care sooner, not later.
You cannot count on the NIH to fund innovative research that leads to effective treatments and disease credibility. The financial resources allocated to fibromyalgia in 2023 amounted to 8 cents per patient.
AFSA doesn’t operate like NIH and here are four key distinctions:
- We do not allow any administrative overhead, and we greatly limit investigator salaries as well as equipment costs. Awarded projects must be budget conscious.
- Funded studies must have the potential to impact the lives of patients within the next five years. They need to be focused on treatments, or uncovering mechanisms that either lead to better therapies or diagnostic markers.
- We toss out applications that focus on exercise, psychosocial issues, or patient self-help.
- We are an all-volunteer organization. Our only incentive to remain in operation is to come up with a cure … at the very least, biomarkers and effective treatments.
Unlike government institutions that feed off your tax dollars, AFSA relies on public support to fund studies. Our sole mission is to help patients get the quality care they deserve, but we need your help.
Make a Difference

While our website provides free patient education, money is required to accelerate the pace of research discoveries. Help us build on the successful momentum of recently funded projects. There are many ways to assist:
- Direct contribution (one time or monthly), either online or via check.
- If you, your significant other, or a family member is employed with a large corporation, ask about employer sponsored payroll giving programs. Many of these programs will also match donations. Companies may have their own system or they might use other programs such as Benevity, YourCause, or CyberGrants/Frontdoor … to name a few.
- In addition to employer sponsored programs, many companies use workplace giving platforms such as America’s Charity or Network for Good. It may be easier to donate tax-free a small amount through payroll deductions.
-
Ask friends and family to donate in your honor in lieu of a holiday gift or birthday present. Our online and printed contribution form accommodates honorarium giving.
If you have a question about employer sponsored or giving programs, please email us at afsa@afsafund.org. The same holds true for donating securities.
If you or family members are concerned about AFSA’s credibility as a charity, we have a 4-star rating from Charity Navigator. We also have a Platinum Seal of Transparency from Guidestar/Candid, the largest nonprofit oversight organization in the world.
Stay Current on Treatments & Research News: Sign up for a Free Membership today!
Fibromyalgia Research Update References
1. Agarwal A, et al. Physicians’ knowledge, attitudes, and practices regarding fibromyalgia. Medicine 103:31(e39109), 2024. Free Report
2. McGhie-Fraser B, et al. Validation of the Persistent Somatic Symptom Stigma Scale for Healthcare Professionals. J Clin Epidemiol. 174:111505, 2024. Free Report
3. Lofgren M, et al. The effects of a 15-week physical exercise intervention on pain modulation in fibromyalgia. Neurobiol Pain. 13:100114, 2023. Free Report
4. Bernardy K, et al. Cognitive behavioral therapies for fibromyalgia. Cochrane Database Syst Rev. 10(9):CD009796, 2013. Free Report
5. Marker Maps Fibromyalgia Pain
6. Is Fibromyalgia an Autoimmune Disease?
7. Targeting the Gut
8. NIH Report – Enter “Fibromyalgia” to get Research Funding for Fiscal Year 2023
