Treatment & Research News
Marker Maps Fibromyalgia Pain
Home | Treatment & Research News

A marker that maps painful body areas could validate the widespread nature of fibromyalgia. One promising molecule is TSPO (translocator protein).
TSPO appears on the surface of many immune cells, but only under certain conditions. It acts like a flag, signaling that the cell is actively fighting inflammation. Marco Loggia, Ph.D., from Harvard Medical School, discussed TSPO’s potential role in detecting inflammation and pain.* In particular, he described how researchers are testing this marker for mapping fibromyalgia and related chronic pains.
Neuroinflammation
To grasp TSPO’s significance, you first need to understand neuroinflammation. This term describes ongoing inflammation in the central nervous system (brain and spinal cord). The key players are glial cells, which are constantly on the lookout for any signs of danger. In healthy individuals, these cells quickly eliminate threats to the nervous system and then revert to their surveillance mode.
“Sometimes these immune responses become problematic,” says Loggia. “Activated glial cells continue unchecked even after the initial threat is resolved. They overstay their welcome and become harmful.” This leads to chronic neuroinflammation, which is linked to diseases like Alzheimer’s, Parkinson’s, and schizophrenia.
TSPO and Brain Imaging
Sampling brain tissue is too invasive. Alternatively, the brain can be imaged using PET (positron emission tomography). PET involves injecting a radioactive tracer that binds to TSPO, producing a signal on the brain scan. In healthy brains, TSPO levels are barely detectable. However, neuroinflammation increases TSPO production, which shows up as hot spots on PET scans.
Loggia studied painful conditions with evidence of neuroinflammation using PET to tag TSPO. Examples included fibromyalgia, low back pain, and migraines. The TSPO hot spots indicate activated glial cells, which may contribute to persistent pain. The location of the TSPO signal is particularly revealing.
Signal Locations
Loggia’s first PET studies using a TSPO tracer were performed on people with chronic back pain. Sometimes, patients showed a strong TSPO signal in the cortex, but not always. Loggia suspected leg pain was the driving force.
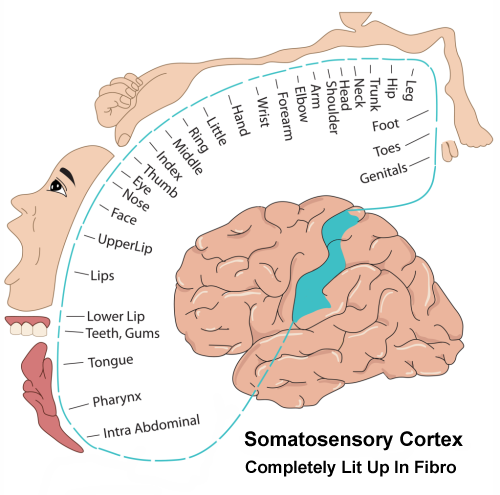
“Comparing patients with leg pain versus spinal pain, those with added leg pain showed a greater signal in the cortex,” says Loggia. He also assessed patients for their “fibromyalgia-like” score. The higher the score (more painful body areas), the greater the signal, particularly in the somatosensory region of the cortex.1
“The somatosensory cortex contains a full representation of the body,” says Loggia. “Different parts of this cortical region process sensory inputs from different body parts.” For low back pain patients, “We saw a TSPO signal elevation in the cortex that matches the regional representation of back and leg pain.”
What about people with migraines? The TSPO signal appears in the cortical area representing the face/head.
Looking at fibromyalgia patients, Loggia says, ”We should see the whole somatosensory cortex light up because patients report widespread pain. And that is what we see.”2 Indeed, Loggia’s finding was replicated by an AFSA-funded study.
No Sex Differences
TSPO is a marker on immune cells, and there are often differences in how the immune system works in men and women. However, Loggia did not see any sex differences in his low back pain studies.
Spinal Cord
So far, all studies relate to findings in the brain. Can TSPO pick up pain in the spinal cord? Yes, Loggia showed TSPO can detect areas of inflammation in the spinal cord of back pain patients.3 It also illuminated the surrounding structures, such as the nerve roots and the dorsal root ganglia (or DRGs). The DRGs contain the cell bodies of nerves just before they enter the spinal cord. While the DRGs reside outside the cord, they are enclosed by TSPO-producing glial cells. More importantly, the DRGs are implicated in contributing to fibromyalgia pain.
Peripheral Cells
“Wouldn’t it be wonderful to use the same marker to image inflammation in the brain, spinal cord, and peripheral tissues like joints?” asks Loggia. Since many immune cells produce TSPO, it might work as a marker outside the nervous system too.
Loggia tested TSPO’s ability to detect inflammation caused by knee osteoarthritis. He examined PET scans of people with and without knee pain due to osteoarthritis. Just like the “hot spots” in the brain that reflected inflammatory pain, the TSPO signal was intense for those with osteoarthritis. Loggia could also tell if patients had arthritis in one or both knees.
While knee osteoarthritis is not fibromyalgia, Loggia’s study reveals two important findings:
- The intensity of the TSPO signal is proportional to the level of knee pain.
- The TSPO signal strength correlates with the concentration of several immune substances in the blood.
This suggests that TSPO may detect pain and inflammation in tissues, although more studies are needed.
Treatment Response
If TSPO can pick up pain and inflammation, it might be useful for measuring physiological responses to treatment. Often, therapies for fibromyalgia don’t pan out because short-term improvements are fueled by hopeful thinking. A tool that objectively tracks improvements in pain after treatment is needed.
For example, in knee osteoarthritis, total knee replacement removes the source of inflammation, yet 30 percent of patients continue to experience pain. Loggia found that TSPO signals in the brain before the knee replacement helped predict response to the surgery.
The pre-surgery signal was more intense for patients who still had knee pain one year later. “This suggests that the TSPO signal we are measuring is not an epiphenomenon,” says Loggia. “It appears to have something to do with the establishment or maintenance of persistent pain.”
High-intensity signals in the sensory cortex reflect the “fibromyalgia-like” nature of the pain. These TSPO signals also depict the degree of neuroinflammation in the brain. As new treatments are developed for fibromyalgia, researchers might first put them to the “TSPO test” or something similar.
Beyond TSPO
Loggia highlights using TSPO as a marker for chronic pain and neuroinflammation. However, detecting TSPO using PET requires injecting a radioactive tracer, which is not ideal. Fortunately, new tools are being developed.
“Many groups around the world are looking at the concentration of brain metabolites believed to be linked to glial cell activity,” says Loggia. In fact, several research teams are focused on fibromyalgia. The next step will be to compare these metabolites with TSPO findings in the same patient. If a substantial overlap exists, these metabolites may be a suitable alternative. But for now, Loggia concludes, “The use of TSPO to image peripheral and central nervous system inflammation (and pain) is opening new doors.”
Stay Current on Treatments & Research News: Sign up for a Free Membership today!
Symptoms | Medications | Alternative Therapies | Muscle Pain Relief | Fibro Friendly Exercises
1. Alshelh Z, Loggia ML, et al. Brain 145(3):1098-1110, 2022. Free Article
2. Albrecht DS, Loggia ML, et al. Brain Behav Immun 75:72-83, 2019. Free Article
3. Albrecht DS, Loggia ML, et al. Pain 159(5)968-977, 2018. Free Article
* Neuroinflammation: Does it have a role in human chronic pain? by Marco Loggia, Ph.D., presented at the International Association for the Study of Pain (IASP) World Congress, August 5, 2024.
