Projects Funded
Understanding Fibromyalgia Flares
Principal Investigator: Nick Fallon, Ph.D.; Andreas Goebel, M.D., Ph.D. (Co-PI)
University of Liverpool, United Kingdom
![]()
When a fibromyalgia flare hits, it’s common to ask: What did I do to cause this? Flares typically last more than three days and occur once a month.1 During this time, all you can do is brace yourself because treatment approaches tend to be ineffective. Until your symptoms level out, you are down for the count (i.e., taking it easy). This project provides a better understanding of the biochemical causes of your fibromyalgia flares.
Contributing Factors
Flares are debilitating and life-disrupting, but no one knows what sets them off. Do the pain control mechanisms in your spinal cord give out or are the processes in your brain too scrambled to work properly? Or maybe the key player is a hyperactive immune system that spews out chemicals to make you feel sick.
Identifying what happens during flares will bring researchers closer to understanding what drives your fibromyalgia symptoms through the roof. And that’s the focus of this AFSA study.
Neuroimaging expert Nick Fallon, Ph.D., in collaboration with Andreas Goebel, M.D., Ph.D. (pain immunologist), form a unique team to sort out what happens during flares. “We hypothesize that fibromyalgia flares are associated with alterations in brain function and with an activation of the adaptive immune system,” says the two investigators.
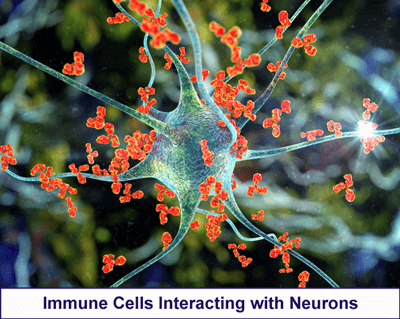
Your adaptive immune processes release chemicals (such as cytokines) and antibodies to attack and destroy foreign invaders. Once the threat is neutralized, this system retains a memory of the invader in case it tries to strike again. Of course, a defect in this chain of events often leads to autoimmune diseases. A prior study by Goebel shows that fibromyalgia patients produce antibodies that attack the satellite glial cells or SGCs.2 The SGCs surround the neurons–or ganglia–at the entrance to the spinal cord and can increase the intensity of the incoming signals.
While traditional autoimmune diseases cause visible damage (such as joint destruction), this is not the case for fibromyalgia. Instead, researchers suspect that the antibodies around the SGCs are ramping up the pain signals entering the cord. No tissue destruction is visible, but the pain and other symptoms caused by the attack are very real.
Expectations
Multiple abnormalities in the way the brain, spinal cord, and immune system function in fibromyalgia are well documented. But in every published report there is tremendous variability. That’s because these studies only take a snapshot of what happens at one point in time. Some patients are probably in a flare up, while others are having a relatively good day.
This study is more like looking at a video than a snapshot. Fallon is evaluating fibromyalgia patients at two time points. First, patients are examined while experiencing everyday baseline symptoms. Next, patients are assessed during a serious pain and fatigue exacerbation (i.e., a flare).
Fibromyalgia involves a dynamic series of processes that produce the wide-ranging symptoms. Think of it as a team sport, except in this case, victory is the flare that cranks up your symptoms. By examining the difference between baseline and flare episodes, Fallon plans to identify the most valuable player (MVP) on the team. This player (or process) is key to producing your symptoms while the rest of the team just does as they are told.
The brain, spinal cord, and adaptive immune system functions will be assessed before and during fibromyalgia flare episodes. In addition, all subjects will undergo a variety of pain measures at both time points to objectively confirm the significant increase in pain sensitivity. “We anticipate that flare-specific patterns of brain activity and immune activation will be observed,” says Fallon.
Spinal Cord Glitches
The pain inhibitory processes in your spinal cord do a poor job. The cord is supposed to pour out opioids when the body is subjected to pain. However, when fibromyalgia patients are given a painful stimulus, about half of them feel increased discomfort.3 This is the opposite of what should happen.
If you view the spinal cord as one of the players on a team, it appears to be unreliable half of the time. Fallon expects to show that the spinal cord fails to score any points for relieving pain during a symptom flare. In fact, it may just rack up penalties!
Scrambled Brain
Do the brain networks communicate differently in fibromyalgia to cause flare episodes? What about regional changes in gray matter volumes? And how effectively does the brain respond to painful stimuli during fibromyalgia flare ups? Fallon addresses these questions with a neuroimaging technique called a functional MRI (fMRI). In particular, he will compare fMRI scans of patients during baseline and peak symptom flare conditions.
Other brain imaging studies in fibromyalgia patients show unhealthy communications between certain brain centers. “Differences in the brain are now known to be associated with pain intensity reported on the day of testing,” says Fallon. So, during flare episodes, Fallon suspects this communication “chatter” among some brain networks will be worse.4 Commenting on this, “No research studies have ever evaluated brain function in fibromyalgia during a flare and compared it to baseline function.”
Immune System’s Role
The immune system’s role in fibromyalgia consists of many players. Looking at any one player won’t give you the score on what is happening to cause fibromyalgia flares. So, Goebel is assessing the following suspects to determine which one is likely to be the team’s MVP:
Cytokines – These substances are increased when the immune system is activated, and many are elevated in fibromyalgia.5 Several cytokine concentrations are expected to increase during symptom flares.
GFAP – This marker of inflammation is released by glial cells – both the satellite glial cells (SGCs) surrounding the neurons entering the cord and the glial cells in the brain. Prior studies (including one funded by AFSA) show neuroinflammation throughout the brain in fibromyalgia patients. Goebel is analyzing GFAP in the serum to determine if it tracks with symptom severity. He suspects when patients are in a flare, this player will score more pain and fatigue points.
Anti-SGC Antibodies – When the antibody-portion of the serum from fibromyalgia patients is injected into mice, antibodies are found attacking the SGCs. “Increased concentration of these antibodies are expected during flare episodes in fibromyalgia patients,” says Goebel.
B Cells – These cells are important players in the body’s adaptive immune response. They produce antibodies that kill infectious agents. B cells can also become overly sensitized. In fibromyalgia, this means changing the function of the cells they attack rather than destroying them. It’s like a team player that gets carried away, doesn’t follow the rules, and knocks other teammates down. Goebel suspects B cells will be more active and possibly more sensitized during flare episodes in fibromyalgia patients.
General Hypothesis
When the video reels of the fibromyalgia team players at baseline and during flares are compared, what do Fallon and Goebel expect to see? They suspect the MVP will be enhanced B cell activity. Increased antibody concentrations (anti-SGC antibodies) and cytokines will assist the MVP to score points. These immune system players will signal the spinal cord and brain to get more involved in the game of making fibromyalgia patients feel awful.

Study Design
Twenty fibromyalgia patients will be followed over an 18-month period. A cell phone app will chart their daily symptoms of pain and fatigue to detect when they are in a flare episode. A flare episode is defined as an increase in symptom scores of roughly a 30 percent for a minimum of three days.
Prior to the flare, patients will undergo a battery of testing, and the tests will be repeated when patients are in a flare episode. Brain imaging data, spinal cord processes, and immunological functions will be compared for each patient at baseline and during the flare.
Potential Benefits
“Investigating symptom flares will provide unique insight into what causes a person’s fibromyalgia symptoms,” says Fallon. This study will highlight which players (or processes) make the symptoms worse, and which players are just along for the ride.
“For the first time, brain scans and immunological investigations are being carried out during a flare in fibromyalgia patients,” says Fallon. “This allows for a correlation between the neurological and immune systems. It also addresses the disease dynamics.”
“This study can uncover potential biomarkers to aid in the early recognition and diagnosis of this disease,” says Goebel. Although if promising markers are found, he says larger-scale studies would be needed to validate them.
How might a biomarker fit into the team sports analogy? Consider it to be the equivalent of a “set play” or strategy that scores points at least 95 percent of the time. And in the case of fibromyalgia, it’s the factor that causes your flares.
Fibro Flare Players
This funded project looks at all the possible players that contribute to causing fibromyalgia symptom flares.
Learn how your immune system conspires with your central nervous system (spinal cord and brain) to generate your slew of symptoms. Read more.
On the other hand, here are individual articles on the cast of characters:
Satellite Glial Cells (SGCs) – immune cells located just outside the spinal cord appear to be under attack and this can increase the intensity of sensory signals
Glial Cells – microglia and astrocytes are two types of glial cells in the brain and spinal cord that are activated to produce symptoms in fibromyalgia
Spinal Cord – the pain filtering system in your cord doesn’t work properly in fibromyalgia
Brainstem – this midlevel player between the cord and the brain that should shut down your pain but it does a poor job
Brain – your brain is ultimately in charge of reducing your symptoms but it is ineffective because there is too much chaos in the brains of fibromyalgia patients
How do you counter so many players that make you miserable? Here are links to treatment-related pages to help keep you out of flare ups:
Medications | Alternative Therapies | Muscle Pain Relief | Fibro Friendly Exercises
But if you are in the midst of a flare, here are articles to help you get through it:
Self-Help Strategies | Managing Pain | Reducing Fatigue
Want to see more studies like this? Help AFSA fund more research.
References for Understanding Fibro Flares
- Gomez-Arguelles JM, et al. Reumatologia 60(4):242-246, 2022. Free Report
- Goebel A, et al. J Clin Invest 131(13):e144201, 2021. Free Report
- Potvin S, Marchand S. PAIN 157(8):1704-1710, 2016. Abstract
- Fallon N, et al. PLOS ONE 11(7):e0159198, 2016. Free Report
- O’Mahony LF, et al. Rheumatology 60(6):2602-2614, 2021. Free Report
