Fibromyalgia Basics
Fibromyalgia Headaches
… treatments to ease your pain
Tension-type and migraine headaches, along with ear and eye pain as well as jaw and facial discomfort are common symptoms. Yet, medications for head pain often disappoint because they don’t fix the knots in muscles that contribute to your fibromyalgia headaches. These firm nodules, called myofascial trigger points (MTPs), are treatable. In fact, studies show your horrendous head pain is primarily due to MTPs in only six sets of muscles.
More than 70 percent of people with fibromyalgia have chronic headaches. If neck pain is added, this figure approaches 100 percent. Unfortunately, the nature of your symptoms is misleading. Severe shooting pains and throbbing sensations (often with twitching around the eyes and face) are typically neurological signs. However, MTPs contain chemical reservoirs that irritate nearby nerve endings, which explains these neurological symptoms.
What Are MTPs?
Before diving into relieving headaches related to MTPs, what are these nasty pain generators? They feel like firm nodules in the muscles. When you press on MTPs, they hurt and radiate pain. MTPs occur in tight ropy muscle bands and represent an area where the fibers are contracted or bunched up. They restrict range of motion and cause muscles to fatigue four times faster than normal.
There are two types of MTPs: active and latent. The active versions are the primary source of your discomfort because they hurt all the time (you do not have to press on them). Conversely, latent versions occur in every one and only hurt when pressed.
Almost all fibromyalgia patients have active MTPs in their trapezius muscle and they are strongly tied to headaches. In fact, the more MTPs you have, the greater your pain severity. So, treating MTPs leads to less overall fibromyalgia pain, as well as the frequency and intensity of your headaches.
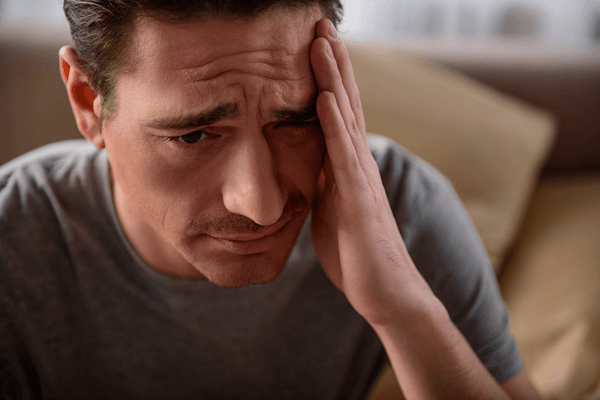
Tension Headaches
Tension headaches occur in everyone, but more so in people with fibromyalgia. They feel like the whole head hurts, but the muscles most likely affected are the upper trapezius, sternocleidomastoid, temporalis, and suboccipital. Two other sets of muscles involved in headaches are the splenius capitis and splenius cervicis. These muscles travel along your cervical spine and attach to the base of your skull. Figures 1 – 6 illustrate how the MTPs in each of the six muscles generate head pain.
Is there a difference between people who chronically experience tension-type headaches and those who don’t get them? Yes, according to studies by Cesar Fernandez-de-las-Penas, Ph.D., of Spain. He examined the upper trapezius, sternocleidomastoid, temporalis, and suboccipital muscles for MTPs in both subject groups.1 Close to 65 percent of the headache patients had active MTPs in the four muscles, while they were not detected in the controls. In addition, patients with active MTPs were prone to more severe headaches than patients without MTPs on the exam day.
But how can one be sure that active MTPs in the muscles are linked to the head pain the patients feel? When the MTPs in all six muscles in figures 1-6 are pressed, headache patients say, “Yes, that’s my pain!”2 On the other hand, injecting a salt solution into the MTPs in healthy controls makes them say, “That gives me a headache.”
Headache Frequency
What is the difference between people who get headaches almost every day and those who get 5-10 per month? Both the chronic and episodic headache groups show the same number of active MTPs.3 However, the head pain intensity does not correlate with the presence of MTPs in the episodic group. Researchers suspect the MTPs in chronic headache patients bombard the central nervous system with painful inputs. The net result is a spreading of pain, a lowering of the pain threshold, and an increased headache frequency.4 This process, termed central sensitization, is not present in people with episodic headaches.
A state of central sensitization already exists in people with fibromyalgia, which could be why you have chronic headaches. With the lowered pain thresholds, it doesn’t take much for the MTPs to produce excruciating headaches in fibromyalgia patients.
Migraines
Migraine begins with a triggering event that causes the cell membranes surrounding the brain to become hyperexcited. Eventually the trigeminal nerve, which supplies all the muscles in the face and head, becomes irritated and leads to throbbing migraine pain and other symptoms. Could it be that active MTPs in the neck/head muscles operate as the “triggering event” in people with migraines?
To answer this question, patients with one-sided migraines were evaluated for MTPs in the four neck/head muscles depicted in the figures 1-4. Researchers found active MTPs on the side that the migraine always occurred, but none on the other side.5 In fact, pressing on the MTPs generated a pain pattern patients recognized as their migraine. Researchers suspect that MTPs in the head/neck irritate the trigeminal nerve and contribute to the initiation and perpetuation of some migraines.
Migraine patients exhibit MTPs in the neck and head muscles, especially in the trapezius and temporalis.6 In addition, injecting the MTPs with lidocaine reduces the severity and frequency of migraine attacks.7 However, it may not completely resolve migraines because they are more complicated than tension headaches.8
Headache Self-Help
Look at figures 1-6 to determine which MTPs contribute to your headaches. Then apply finger pressure to deactivate the trigger points. Use a tennis ball for the back regions by placing it between you and the floor or wall. Alternatively, a Thera Cane allows you to press on trigger points all over your body. Just don’t press so hard as to cause pain – this traumatizes the muscle and causes more MTPs. See Identifying & Treating Trigger Point Pain for more advice.
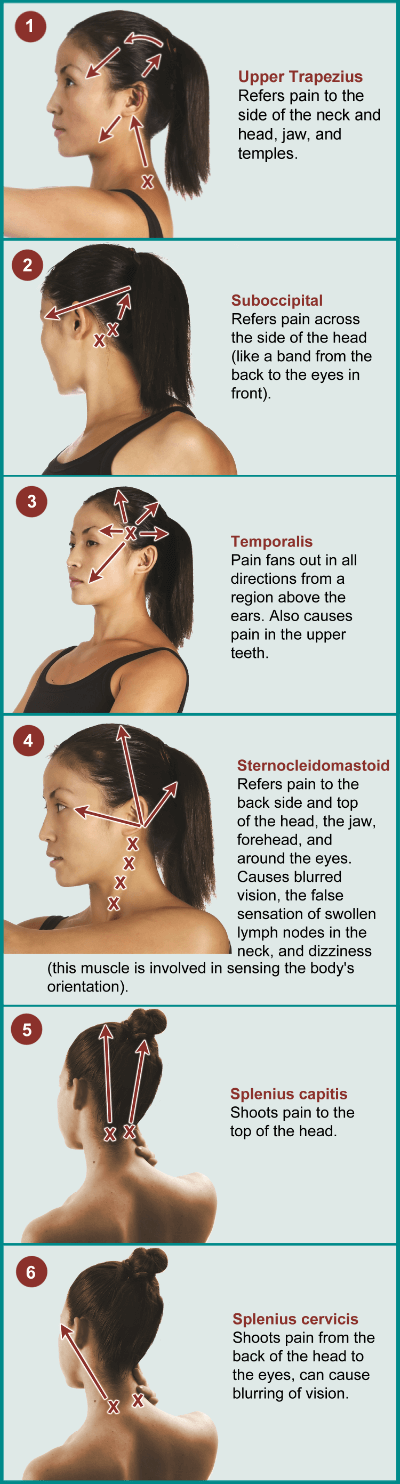
One example for deactivating the MTPs at the base of the skull near the splenius capitis is illustrated in figure 7. Move your thumb in a circular motion to massage the MTP. Always stay hydrated to flush out the chemical toxins released by the MTPs. Otherwise, the muscle fibers will bunch back up again.
Therapies for deactivating MTPs were developed for people who only have regional pains. Fibromyalgia patients have a sensitized nervous system, so pressing on headache-related MTPs may hurt more. To reduce the hurdle of treatment discomfort, try the following approaches before and after pressure application:
Apply moist heat. A neck/shoulder heat wrap is ideal to use before and after any treatment. Heat relaxes muscles and improves local circulation (to carry away chemicals released by the MTPs).
Use a topical anesthetic. Coolant gels and roll-ons work as topical anesthetics to reduce the pain caused by pressing on MTPs. Examples include Orthogel (gel is $10; roll-on is $34) and Biofreeze (gel is $14; roll-on is $32). Both are available on Amazon. Another option is lidocaine spray for $10 at your local drugstore.
Beneficial Stretches
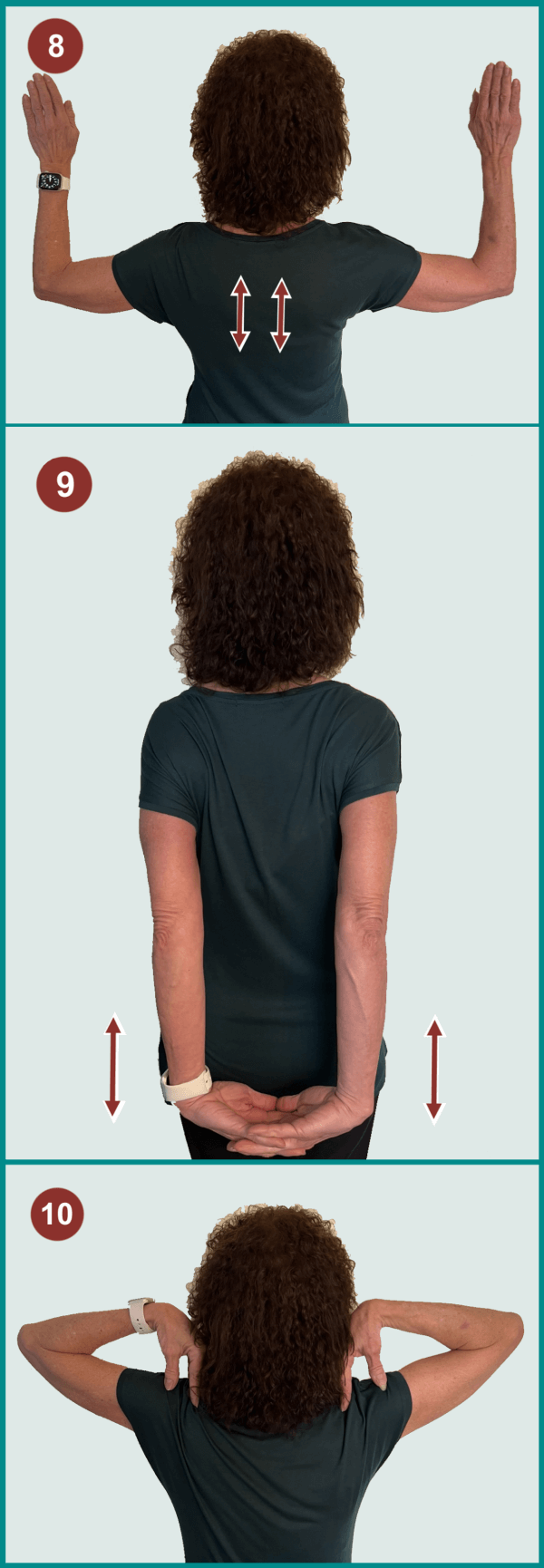
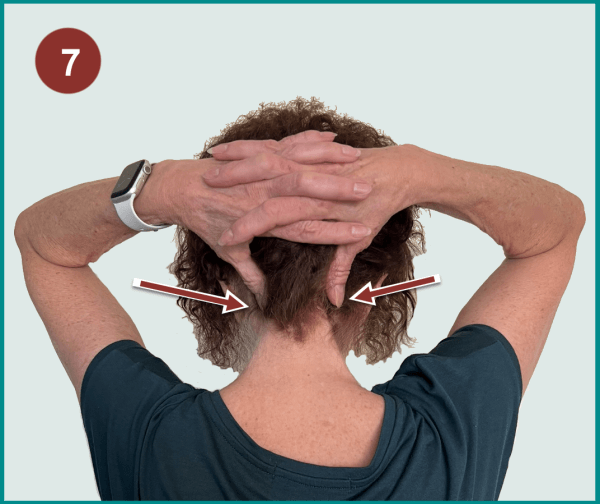
MTPs cause muscles to shorten and restrict your range of motion. So, keep your neck and shoulder muscles elongated and relaxed to minimize the development of MTPs. Try incorporating the following simple stretches into your daily routine:9
Scapular Training – MTPs occur more commonly in the upper half of the trapezius muscle than they do in the lower portion. As a result, the top part feels like a brick while the lower half becomes chronically stretched and weak. This movement helps balance the load and strengthens the lower portion (see figure 8). First, open your chest and rotate your palms outward. Second, move your scapula up and down several times.
Pectoral Stretching – This maneuver loosens up tight chest muscles (see figure 9). First, open your chest and interlock your fingers behind your back. Second, pull your hands downward.
Shoulder Loosening – First, place hands on top of shoulders (see figure 10). Second, move elbows around slowly in large circles.
Medical Assistance
Manual therapies and dry needling that target MTPs are effective for tension headaches and migraines.10
Spray and Stretch – Many physical therapists use this technique with a Fluori-Methane coolant spray. Muscles with MTPs are shortened in length because the fibers are taut or contracted. This technique is designed to stretch a muscle to release the MTPs and improve range of motion. First the therapist sprays the surface, then anchors one end of the muscle while gently stretching it. The procedures should not be painful, so let your therapist know if they are being too forceful.
Massage – Many forms of massage can deactivate MTPs. One study shows regular massage of the neck and shoulders for 15 minutes significantly reduces pain in fibro patients.11 These two areas contain MTPs in fibromyalgia, so massage should decrease the number and intensity of your headaches.
Manipulation – There are lots of little joints along the spine, called facets, that may be involved in developing some MTPs. As a result, spinal manipulation can relieve MTP pain.
Dry Needling – Acupuncture needles are inserted into the eye of the MTP to release the trigger point. Physical therapists usually perform this technique, except in five states: California, Hawaii, New York, Oregon, and Washington. In these states, you must visit a licensed acupuncturist. Regardless of which specialist you see, call around to ask if they dry needle MTPs before booking an appointment.
Preventive Care
Bear in mind that MTPs quickly return if the underlying factors that encouraged their development are not addressed. Hypothyroidism and low levels of vitamin B1 and B6 promote the development and perpetuation of MTPs.
Another reason MTPs rapidly return is due to the central pain state of fibromyalgia. MTPs can fuel your central nervous system dysfunction, and the opposite is also true. The aberrant central nervous system in fibromyalgia may contribute to the development of MTP-related headaches. Therefore, maintain a daily program to keep troublesome MTPs in check.
Tension headache medication works best if you take it before the head pain gets bad. Example medications include ibuprofen (400 mg) and aspirin (500-1,000 mg). Researchers speculate that taking these drugs right away reduces the spread of pain, thereby minimizing your discomfort.12
Migraine medications include a long list of drugs, such as divalproex, topiramate, metoprolol, and amitriptyline. However, many patients avoid using these agents due to unwanted side effects. Another option with less side effects is 3 mg of melatonin one hour before bedtime.13 It has potent anti-inflammatory and antioxidant properties, and the blood levels of this hormone are low in migraine patients. Several studies show melatonin reduces the frequency and intensity of migraines with no adverse effects.
AFSA funded three projects in 2024. Help us fund more in 2025!
Read more about myofascial trigger points (MTPs) in our section on Muscle Pain Relief. Learn about other Symptoms, Medications, and Alternative Therapies.
Stay current on Treatment & Research News. Sign up for a FREE Membership.
References for Fibromyalgia Headaches
- Fernandez de las Penas C, et al. Headache 46:1264-1272, 2006. Abstract
- Arendt-Nielsen L, et al. Clin J Pain 32(8):711-718, 2016. Abstract
- Fernandez de las Penas, et al. Manual Ther 11(3):225-230, 2006. Abstract
- Fernandez de las Penas C, et al. Cephalalgia 27(5):383-393, 2007. Abstract
- Fernandez de las Penas C, et al. Cephalalgia 26(9):1061-1070, 2006. Abstract
- Palacios-Cena M, et al. Pain Med 18:2485-91, 2017. Free Report
- Fernandez-de-las-Penas Curr Pain Headache Rep 19:28, 2015. Abstract
- Ferracini GN, et al. Clin J Pain 33(2):109-115, 2017. Abstract
- Adachi K, et al. BMC Neurology 24:316, 2024. Free Report
- Fernandez-de-las-Penas C, et al. Int J Environ Res Public Health 17:4126, 2020. Free Report
- Nadal-Nicolas Y, et al. Int J Environ Res Public Health 17:4611, 2020. Free Report
- Fernandez-de-las-Penas C, et al. BMC Neurology 20:43, 2020. Free Report
- Nelakuditi B, et al. Cureus 12(10):e72559, 2024. Free Report
