Possible Causes
Hyped-Up Ganglia
Before any signal enters your spinal cord, there is one last stop where it can be influenced: the dorsal root ganglia (DRG). The DRG are bulb-shaped structures containing the cell body of each neuron and they are surrounded by a glial cell (called a satellite glial cell or SGC). The DRG/SGC complex can sample information from the blood and lymph and use it to influence the CNS.
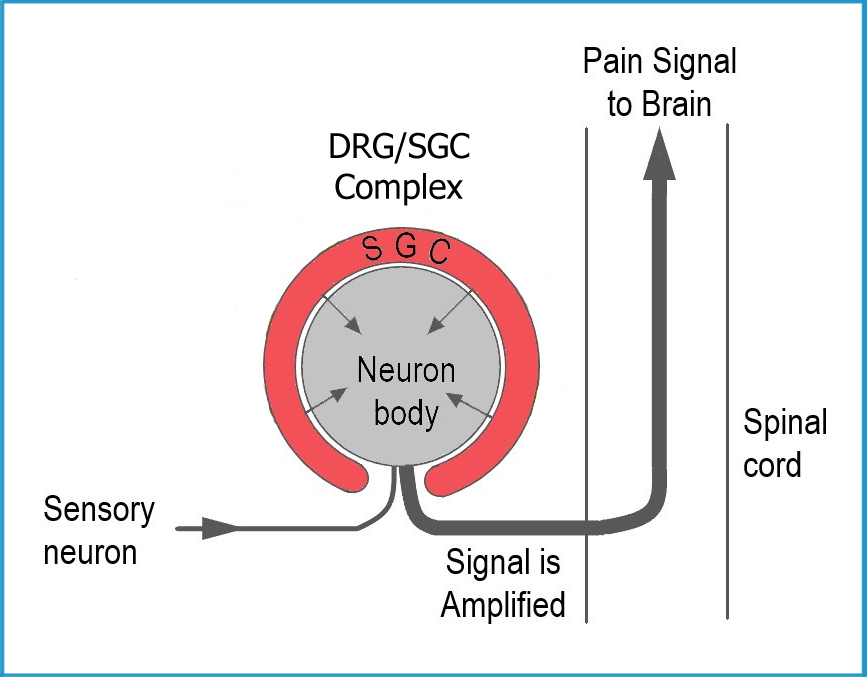
If the DRG/SGC get distress signals from the periphery, such as an injury, an infection, or something else that the brain needs to know about, it can convey that information to the cord. Just as the cord can modulate the signals headed up to the brain, the DRG/SGC complex can tone down signals with GABA or amplify them with substance P (and other pain transmitters).
What makes these structures interesting is that the fluid space between the DRG and the surrounding glial cell is shared with the cerebral spinal fluid in the cord. So, it is uniquely positioned to balance the information from the CNS with that of the periphery.
For decades, the DRG/SGC complex was ignored in fibromyalgia research. Understandably, these structures cannot be analyzed by modern neuroimaging … at least not in humans. However, scientists started to get creative, injecting mice with various blood cells from fibromyalgia patients to see what happened. As it turns out, the transfer of fibromyalgia cells to mice caused a dramatic drop in pain thresholds and the DRG/SGC structures may be responsible.
Unlike humans, the DRG/SGC can be imaged and the strength of the signal generated by this unit can be measured before and after giving the mouse a pain stimulus. In addition, these transfer studies in mice allow researchers to look at how the DRG/SGC are impacting the function of the CNS. For example, are the DRG the source of the three to fourfold increase in substance P, nerve growth factor, and brain derived neurotrophic factor in the spinal fluid? It’s possible but this avenue has not been explored.
A closer look at the DRG/SGC as well as other processes in the peripheral organs/tissues may lead to a better understanding of why the CNS is so dysfunctional. In turn, this is bound to lead to better treatments for fibromyalgia than those that solely target the CNS.
For now, two passive transfer studies have been published and both highlight the role of the DRG/SGC complex. It’s possible that something in the blood is making the DRGs behave differently, such that the signals entering the spinal cord are chronically amplified. This could make the CNS falsely think that it is fighting a widespread infection or something equally serious. A summary of each study is below.
Immunoglobulins Surrounding the DRG: Could antibodies in the serum of fibromyalgia patients be attacking the glial cells that envelop the DRGs? If this is the case, it would imply that fibromyalgia is a very different type of autoimmune disease. Instead of targeting the joints, muscles or organs, the DRG/SGC complex might be the focus of the immune system’s attack. Read more.
Misbehaving Neutrophils: Transfer to blood cells from fibromyalgia patients to mice led to a rapid drop in pain thresholds in the animals. The neutrophils were identified as the cells causing the pain and they were exerting their effects on the DRGs. It appears that the neutrophils from fibromyalgia patients have undergone changes that can activate the DRGs in such a way as to ramp up pain. This is a promising new area of research, but the study only involved nine patients. Hopefully additional research will explore the role neutrophils play in producing fibromyalgia symptoms.
