Projects Funded
Genetic Influences on the Pain Control System
Principal Investigator: Serge Marchand, Ph.D.
University of Sherbrooke, Quebec, Canada
(October 2009)
The pain control system operates on the basis that pain inhibits more pain. When a person is first subjected to a noxious stimulus, this system releases pain-relieving substances into the spinal cord to reduce the impact of additional discomfort. In a prior AFSA-funded study, Marchand showed that the pain control system didn’t work well in fibromyalgia, but he stressed that there was a lot of variability.1
“Some healthy subjects have a very strong pain modulation system and others have such a weak one,” says Marchand. “If we did not know better, we would think that they were fibromyalgia patients. There are likely certain genetic predispositions that determine the strength of a person’s pain inhibitory system.”
The pain inhibitory controls use serotonin, norepinephrine, and dopamine transmitters that cause the release of opioid-like pain relievers. Given that fibromyalgia patients have double the normal concentration of opioids in their spinal fluid, the faulty pain system is probably not due to an inability to produce opioids. Therefore, the focus of the genetic abnormalities was placed on serotonin and dopamine, and both were examined in relationship to the strength of the subject’s pain control system function.
Dopamine Link
Dopamine activity in the brain is greatly increased in healthy subjects given a painful stimulus, but not in fibromyalgia patients.2 Ordinarily, the dopamine released would act on a dopamine receptor, which in turn would then lead to the secretion of opioids to produce analgesia. Although there are different types of dopamine receptors, subtype 3 or DR3, was shown by brain imaging to be involved in fibromyalgia.
A genetic mutation can alter the sensitivity of the dopamine 3 receptor (DR3). A less sensitive receptor would require more dopamine to produce the same analgesic results (i.e., release of opioid-like pain relievers).
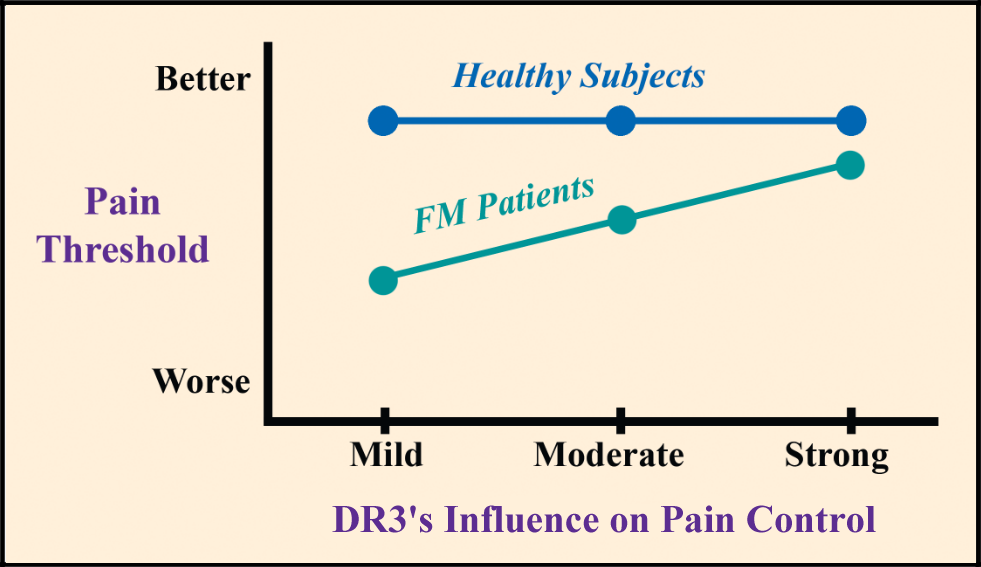
There are three forms of DR3 in people and each produces a varying degree of pain inhibition. One DR3 form leads to “mild” activation of the pain control system, while the other two produce “moderate” and “strong” system activations.
Marchand compared the prevalence of each DR3 form in a group of 37 fibromyalgia patients and 36 healthy control subjects, but there was no difference. 3 In other words, fibromyalgia patients were not more likely to be saddled with the DR3 form that produces milder pain system activation. He also measured the participants’ thermal pain threshold to see if it might be influenced by the strength of the DR3.
It didn’t matter whether the healthy subjects had a dopamine receptor that produced a “strong” or “mild” pain control response, their pain thresholds were the same. However, this was not the case for the fibromyalgia patients. The “strong” version of the DR3 in people with fibromyalgia led to a higher (better) pain threshold than the “moderate” and “mild” versions.
Why might there be a difference between the fibromyalgia patients and the controls? People with fibromyalgia have a hyperactivity problem in their spinal cord, which means that the pain control mechanisms in their spinal cord are already overloaded. Giving fibromyalgia patients genetics that further impairs their pain processing system can tilt the scales to lead to more pain.
“If you are not in pain, alterations in the dopamine receptor will not change anything because you still have some pain inhibitory system function,” says Marchand. “However, if you are in pain, it makes a big difference and you need more pain control function.”
Serotonin … a Mixed Bag
The genetic influences of serotonin on the pain control system are less straightforward than that of dopamine. After serotonin is released at the nerve junction, the body has transporter molecules that latch onto serotonin and carries it back across the nerve junction. It is a way of reusing serotonin repeatedly, if needed. In fact, this is how selective serotonin reuptake inhibitor drugs work, such as duloxetine.
The efficiency of the body’s serotonin transporter system is genetically influenced. Marchand looked at a genetic abnormality that leads to a reduced efficiency of the transporter, such that less serotonin gets recycled for the pain control system. However, a less efficient serotonin transport gene did not alter the pain control system or pain thresholds in the fibromyalgia patients tested.4
In the early years of fibromyalgia research, raising serotonin was the goal. This is why drugs like duloxetine and Savella (which also raise norepinephrine) are thought to be helpful. And for some patients, increasing serotonin may reduce pain. However, Marchand points out in his published study that serotonin can be a pain-reliever and a pain-amplifier.
Some cells in the central nervous system will look at serotonin and ramp up your pain levels. Other cells will look at serotonin and calm down the pain signals. Serotonin’s influence on your fibromyalgia pain is truly a mixed bag, and this transmitter is not likely to hold the key to your treatment success.
- Julien N, Marchand S, et al. PAIN 114:295-302, 2005.
- Wood PB, et al. Eur J Neurosci 25:3576-82, 2007.
- Potvin S, Marchand S, et al. J Pain 10(9):969-75, 2009. Journal Report Click PDF
- Potvin S, Marchand S, et al. Eur J Pain 14(7):742-6, 2010.
