Projects Funded
Detecting Brain Inflammation Using PET
Principal Investigator: Jarred Younger, Ph.D.
University of Alabama at Birmingham
Project findings are published; see Study Update below.
Most people think of their brain as being full of neurons, but the microglia are immune cells that outnumber the neurons. The microglia play an essential role in protecting the brain from any threat, such as a virus or injury. When these cells get a whiff of anything that may harm the brain, they morph into an activated state to fend off infections or repair neurons. Researchers call this an inflammatory state because the microglia release inflammation-promoting chemicals.
Ordinarily, your microglia are activated for very short durations; it’s just a temporary state until the threat is neutralized. During this activated state, they release substances (e.g., cytokines) that cause symptoms of pain, fatigue, sleep disturbance, and brain fog. If the microglia are trying to kill a virus, they release chemicals that harm the neurons in the short-term. Once the threat is gone, the microglia repair damaged neurons, and the nasty symptoms go away.
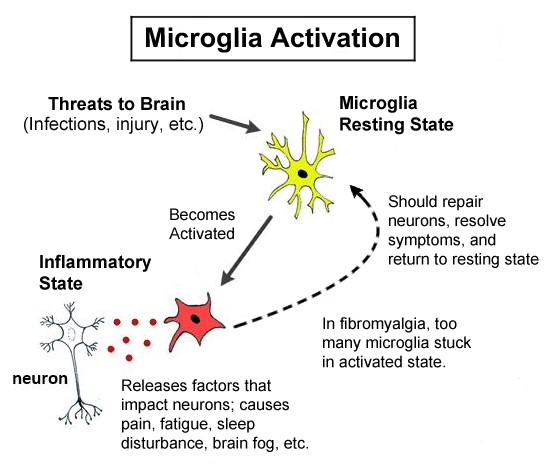
Activated microglia in the inflammatory state produce many of the symptoms found in people with fibromyalgia. In fact, the similarity between microglia in the inflammatory state and fibromyalgia is the basis for this AFSA-funded study by Younger. In fibromyalgia, the microglia may be “stuck” in the activated or inflammatory state rather than being transiently activated as needed.
Study Design
“An excessive number of microglia in the inflammatory state is a known indicator of neuroinflammation,” says Jarred Younger, Ph.D. Microglia in the activated or inflamed state produce a substance called translocator protein (TSPO). This protein appears as a signal on surface of the microglia and it can be detected with brain imaging.
Test subjects are first injected with a tracer that latches onto the TSPO “flags” produced by activated microglia. The tracer generates a fluorescent signal, which shows up on brain scans using positron emission tomography (PET). After the tracer is injected, subjects undergo a PET scan to measure the number and location of activated microglia. Younger will use a newly developed tracer called radioligand [18F]DPA-714.
Tracers that tag the TSPO receptor have been around for years, but they have two drawbacks. First, they quickly pass through the body (half is gone in 20 minutes) and the imaging procedure proposed by Younger takes 30 minutes to complete. Second, the old tracers are not specific enough to only latch onto the activated microglia. They also bind to other brain cells, casting doubt over data interpretation.
Younger’s university developed a longer-acting tracer that sticks around for 110 minutes, providing ample time to accurately obtain imaging results. It’s also more selective at tagging microglia so that the data will hold up to more scrutiny. “We are now in an excellent position to use this process in fibromyalgia,” says Younger about the tracer developed by his radiology colleagues. “Doing so may provide the clearest, most robust, and replicable view of fibromyalgia pathophysiology to date.”
Fifteen fibromyalgia patients were assessed for pain thresholds and degree of severity of all major symptoms for this condition. Ten healthy, symptom-free controls were used for comparison. Younger’s study should form the foundation for future research studies in fibromyalgia by highlighting the microglia’s role.
Study Update
Brain Inflammation Confirmed
“This study shows that fibromyalgia involves a low level of neuroinflammation that is spread across multiple regions of the brain,” says Younger.* More specifically, a larger portion of the microglia are activated in fibromyalgia patients compared to healthy controls.
But how did Younger determine that the microglia were the cells responsible for driving neuroinflammation? “When the microglia are in an inflammatory state,” says Younger, “they absorb more of the chemical tracer we inject into the study participants, called DPA-714. By using a PET scanner, we can measure how much of the brain’s microglia are absorbing DPA-714 and therefore the relative quantity that are in an activated or inflamed state.”
Thirty-four brain regions were assessed for microglia activation. Most areas showed a mild to moderate level of increased activity, indicating inflammation. Of particular interest were areas in the parietal lobe.
Why is the parietal lobe important? “This is where the sensations of the body are integrated and interpreted,” says Younger, adding that this includes the experience of both pain and fatigue. “Within the parietal lobe is a region called the somatosensory cortex, and it processes pain signals coming from everywhere in the body. Neuroinflammation in the parietal lobe would very likely cause enhanced pain processing.”
Perhaps it is no surprise that Younger was able to show significant correlations between the level of inflammation in the parietal lobe and the following symptoms:
- decreased quality of life
- reduced energy
- greater pain
- more severe cognitive problems
Until a few years ago, the pain and other symptoms of fibromyalgia were explained as being a problem with the way the neurons function in the central nervous system. The microglia were viewed to play a supportive role in nourishing the neurons and removing toxic chemicals from the synapse (the transmitting space between neurons). However, activated microglia can be like a thorn in the side of neurons. Whether these immune cells are solely responsible for the symptoms of fibromyalgia, or just making matters worse, is unclear.
Possible Treatments
How does Younger’s finding of neuroinflammation in fibromyalgia impact treatment strategies? Younger says “treatments that can cross the blood brain barrier and push the microglia out of their activated/inflamed state” are needed. One possible medication is low-dose naltrexone or LDN. An AFSA-funded trial of LDN at 4.5 mg/day significantly reduced the pain and related fibromyalgia symptoms in one-third of patients.** For more details, see the LDN trial and article on Giving LDN Your Best Shot.
Factors that can contribute to microglia activation are stress and sleep disruption, so therapies that relieve these symptoms may be beneficial. In fact, mild movement therapies that incorporate relaxation breathing, such as yoga and tai chi, have been found to ease the impact of fibromyalgia. Ironically, the most potent class of medications to relieve pain are opioids, yet they are strong microglia activators. So chronic use of this class of medications may be detrimental in the long run.
* Mueller C, Younger JW, et al. Evidence of neuroinflammation in fibromyalgia syndrome: a [18F]DPA-714 positron emission tomography study. PAIN. 2023 Oct 164(10)2285-95. Free Journal Report
** Younger J, Noor N, McCue R, Mackey S. Low-dose naltrexone for the treatment of fibromyalgia: findings of a small, randomized, double-blind, placebo-controlled, counterbalanced, crossover trial assessing daily pain levels. Arthritis Rheum. 2013 Feb;65(2):529-38. Free to read but not print.
