Projects Funded
CES for Treating Fibromyalgia
Measuring Brain Function and Symptom Changes
Principal Investigator: Anna Woodbury, M.D., M.Sc.
Emory University in Atlanta, GA
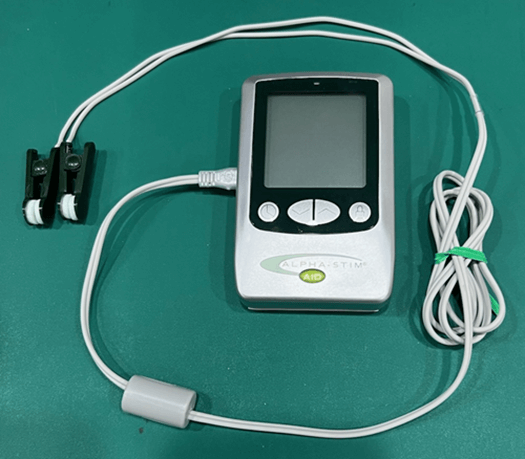
If you haven’t heard of cranial electrical stimulation (CES), you are not alone. It’s a form of brain stimulation therapy that generates a tiny, pulsating electrical current through wire clips attached to the earlobes. The handheld devices are FDA-cleared for the treatment of insomnia, depression, anxiety, and pain. For more details about this device, see our CES article in Nondrug Treatments. Basically, CES is thought to stimulate centers in the brain to improve the way it functions. So, this study test CES for treating fibromyalgia brain abnormalities and improving key symptoms.
A few years ago, pain researcher, Anna Woodbury, M.D., started prescribing CES for her patients with fibromyalgia. “The effects were almost immediate, and not only did individuals report decreases in pain, but also in anxiety and sleep disruption,” says Woodbury. She is affiliated with the Veterans Administration (VA) and her VA center covers the cost of this device … as do many others nationwide.
“Many of my fibromyalgia patients have chemical hypersensitivities and cannot tolerate some of the available drug therapies,” says Woodbury. “So, developing this device as a nondrug treatment for fibromyalgia may present patients with more effective and tolerable options.”
Woodbury is a brain imaging expert and investigating how CES alters brain function intrigued her. Rather than simply measuring the impact CES has on fibromyalgia symptoms and physical function, she designed a treatment trial that includes two forms of brain imaging.
A portion of the imaging analyses and symptom assessments were funded by AFSA as a tag-on to Woodbury’s larger VA-funded study. The AFSA portion is intended to provide a more rounded picture of what CES does for brain function. It also offers insight about the device’s effects on symptoms other than pain, such as fatigue, sleep disorder, and mood. These latter symptoms were not addressed in the VA portion of the study.
Study Design
The initial project funded by the VA tests the effectiveness of CES for treating fibromyalgia patients during a three-month trial. Half the patients were given “active” devices (they emitted the electrical current), while the other half were provided “sham” devices (like a placebo). When the patients turned on the sham devices, they didn’t emit a current. All subjects used the devices for one hour each day.
Prior to using the devices and at the conclusion of the three-month trial, patients underwent multiple neuroimaging tests. Some measured the way brain centers communicated with one another, while others assessed structural and inflammation-related changes. Several studies, including one funded by AFSA, have shown brain inflammation in fibromyalgia patients that correlates with symptom severity. Naturally, it would be helpful to know if CES can reduce brain inflammation.
An array of symptoms and physical function tests were measured in all subjects before and after the CES trial.
Men Included

One-third of the fibromyalgia patients enrolled in the study are men. This is an important aspect of the study because men are generally excluded from fibromyalgia research. Yet, assessing how men and women respond to CES is an amazing opportunity to learn so much more about fibromyalgia.
“To truly understand the complexities of fibromyalgia and develop effective treatments, we must study the condition in both sexes,” says Woodbury. “Ignoring men may lead to an incomplete understanding of the disease. By studying fibromyalgia in both men and women, we can improve our understanding of the diseas’s mechanisms, develop more targeted treatments and enhance the quality of life for all patients.”
Will men respond differently to CES than women? And what about brain function? Does the presence of testosterone in men alter the way their brain’s pain processing centers work? There are enough men in this study to analyze the differences between the sexes. As Woodbury puts it, “Inclusive research benefits everyone.”
VA Portion
How well does CES reduce the pain of fibromyalgia and does it improve physical function? These are the symptom-related questions to be answered by the VA-funded portion of the study.
Assessing how CES might alter the way the various brain centers communicate with one another requires elaborate brain imaging. Woodbury uses a technique called functional connectivity MRI or fc-MRI to measure the brain’s communication networks.
To illustrate the concept of fc-MRI, Woodbury says, “Imagine the brain as a big office building with many departments. fc-MRI is like taking a picture of the building showing which departments talk to each other and how much. It’s like an Inter-Department Communication Map. Functional connectivity refers to how well different parts of the building (or the brain) communicate and cooperate with one another.”
If there is too much connectivity (or communication) between certain areas, it can be like constant chatter or noise in the office. Applying this to brain function, it can lead to the following symptoms:
- increased pain sensitivity
- heightened anxiety
- difficulty focusing
Not enough connectivity (or communication) may mean the brain centers are working in isolation. This isn’t good either and may cause:
- poor coordination of bodily functions
- difficulty processing sensory information
- problems with pain regulation
“In fibromyalgia, the brain communication systems are often off balance,” says Woodbury, like the analogies above. “We are hoping to see if CES can help ‘tune’ this communication to a more balanced state, potentially reducing symptoms.” By using fc-MRI before and after treatment, Woodbury is correlating alterations in brain communication patterns with symptom improvements.
AFSA Portion
Fibromyalgia is more than just a painful disorder. Almost all patients experience profound fatigue and sleep disorder … and for many, depression makes matters worse. The ability of CES to improve this array of symptoms is part of the AFSA-funded portion of the study.
Structural brain abnormalities have also been documented in fibromyalgia patients. Prior studies show that the gray matter volume of the insula is increased in fibromyalgia.1 The insula is tasked with prioritizing all sensory inputs to the brain and is hyperactive in patients with fibromyalgia. Using structural MRI data collected before and after CES treatment, Woodbury hopes to show that the insula’s gray matter volume decreases in fibromyalgia patients. In addition, she will look to see how it correlates with symptom improvements.
Using a different imaging technique (magnetic resonance spectroscopy or MRS), Woodbury is measuring the degree of inflammation in the insula. Many prior studies show inflammation throughout the brain and Woodbury will be looking to see if CES reduces markers of inflammation.2
Aside from looking at brain chemicals linked to inflammation, Woodbury is using MRS to measure the levels of glutamate and GABA. Glutamate is high in the brains of fibromyalgia patients, while GABA is low.3 This imbalance could be due to the activity of the neurons, but it might also be the byproduct of inflammation. Woodbury will determine if these levels “normalize” with CES treatment.
“Going back to the office building analogy, we can think of MRS as an ‘Office Supply Check,’” says Woodbury. “It’s like a system for checking the supplies and air quality in different departments. In fibromyalgia, some departments might have a stockpile or shortage of supplies. Other departments might have poor air quality (reflecting inflammation).”
When inflammation is present in the brain, the immune cells (called the glia) do a poor job of supplying the neurons with nutrients and removing the waste products. This impedes the neurons’ ability to function, leading to congestion in brain transmissions (i.e., poor air quality).
Putting it all Together
Most clinical trials only measure if a specific treatment improves symptoms. Sure, they attempt to determine which symptoms improve and by how much, but Woodbury’s study goes way beyond symptom assessments. Her goal is to try to parse out which changes in the brain correspond to improvements in specific symptoms. Not only that, but she is looking at both men and women with fibromyalgia to see if responses to CES treatment differ between the sexes.
Using the office analogy, “CES treatment might help clear out excess supplies and improve air quality (as determined by MRS brain imaging),” says Woodbury. “By examining both the office supplies and air quality (brain chemistry) and the communication patterns between departments (brain connections based on fc-MRI), we can better understand how CES might help people with fibromyalgia. This could lead to improved treatments and help explain why some people feel better after using CES.”
Combining fc-MRI with MRS imaging technologies offers a more comprehensive picture of how your brain is functioning. It also provides more information about how CES might work to reduce your fibromyalgia symptoms.
If the results of the trial are as impressive as Woodbury’s personal experience using CES for her patients, it will lay the groundwork for larger studies. The end goal is to publish data on how CES works specifically for people with fibromyalgia. Without published guidelines, private insurers and Medicare will continue to deny coverage. At $840 for the device, this is an unacceptable financial barrier for many patients.
Let’s work together to fund more studies like this one!
CES for Treating Fibromyalgia References
1. Puiu T, et al. Arthritis Rheumatol 68(6)1511-21, 2016. Free Report
2. Jung C, et al. PAIN 161(7):1555-1564, 2020. Free Report
3. Foerster BR, et al. Arthritis Rheum 64(2):579-583, 2012. Free Report
