Projects Funded
Biomarkers Expressed on Blood Leukocytes
Principal Investigator: Alan Light, Ph.D.
University of Utah in Salt Lake City
(September 2009)
“One of the critical needs in FMS research is to develop truly objective biomarkers for the disorder,” says Alan Light, Ph.D. “Blood-based biomarkers are especially valuable because they are consistent with traditional medical models, they are viewed as unbiased, and they are relatively low risk for patients (compared to cerebrospinal fluid or tissue sampling markers).”
Light has developed a technique to overcome the obstacle of the blasé blood work in which everything comes back “normal.” Two blood draws were made: after subjects had been resting for a while (at baseline) and then after subjects had performed moderate exercise on a stationary bicycle for 25 minutes (after a stressful challenge).
What does exercise have to do with blood markers and your symptoms? “Muscle pain and both physical and mental fatigue are sensations that a healthy body uses for protection or as a warning signal to prevent overuse of muscles and important areas of the brain,” says Light. “However, in fibromyalgia patients these sensations are overwhelming and unrelenting, and they interfere with normal life activities.”
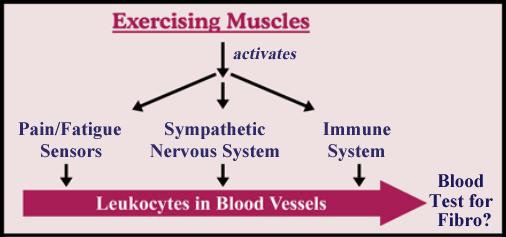
The sensory nerves in the muscles are alongside the blood vessels. Light found that the white blood cells (or leukocytes) are like magnets picking up information from the sensory fibers, sympathetic nervous system, and the immune system (see below). By measuring the leukocyte messenger RNA (mRNA), which contains the genetic blueprints for making what the cells need, Light looked for gene expression test markers.
Baseline Values
At baseline, without provocation, a small group of 18 fibromyalgia patients exhibited substantial elevations in genetic markers for two receptors, P2X4 and TRPV1.1 Both are involved in sensing pain and fatigue in your muscles.2 Although these sensors live on your nerve endings, you have cells in your blood (leukocytes) that know how many of these special detectors your nerves are programmed to make. In fact, your leukocytes can be viewed as spies that contain the genetic blueprints of what is happening in many of your body systems.
Light also found increased genetic markers for an immune system product, IL-10, which fights inflammation and is elevated in people who have disrupted sleep. All in all, three biomarkers were elevated in fibromyalgia patients at rest compared to healthy subjects, depressed patients, and multiple sclerosis patients with extreme fatigue.
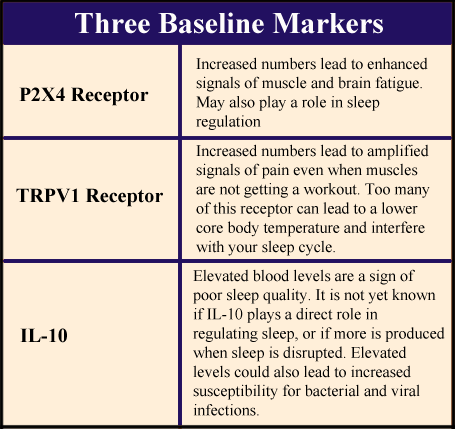
Based on what is known about the P2X4 and TRPV1 receptors, they are likely telling your brain that your muscles are overworked and hurt. They can even trigger signals that lead to abnormal functioning of your peripheral (sympathetic) nervous system and produce a cascade of symptoms that are commonly found in fibromyalgia. The lower levels of physical activity in fibromyalgia cannot be used to explain these results because decreased activity would likely lead to reduced rather than elevated production of these two receptors.
Exercise Challenge
When healthy people perform a half hour of exercise, it’s natural for them to feel a bit fatigued, but these effects are generally gone after 30 minutes of rest. Not unexpectedly, pain, physical exhaustion, and mental fatigue were made worse in patients for 48 hours after the same amount of exercise. Rigorous monitoring of symptoms following exercise documented that overdoing it does magnify the primary symptoms. Although the baseline markers did not get worse, the symptoms did.
“Our graphs clearly show that people with fibromyalgia get worse with exercise,” says Light. “Not only do pain scores increase, but so do the symptoms of fatigue. Post-exercise symptoms have not been thoroughly evaluated in fibromyalgia, but the common assumption that exercise does not exacerbate fibromyalgia is just not true.”
Keep in mind that ideal biomarkers are those that can be demonstrated (and measured) with a simple blood draw at resting conditions. “In terms of marketability, there is no question that baseline markers are what we need,” says Light. “It’s the best way to make the test cost-effective and to be able to get physicians to use it.”
Keeping Tabs on Cellular Function
How does your body sense which cells are getting too much of a workout? All cells operate off of the same energy currency, a molecule called ATP. The more ATP a cell consumes, the harder it is working. The P2X4 receptors in your muscles keep a running tab on how much ATP each cell consumes. It is as though the P2X4 receptor is an abacus for calculating ATP usage. Each ATP molecule consumed by the cell represents a bead on the abacus so a running tally can be kept.
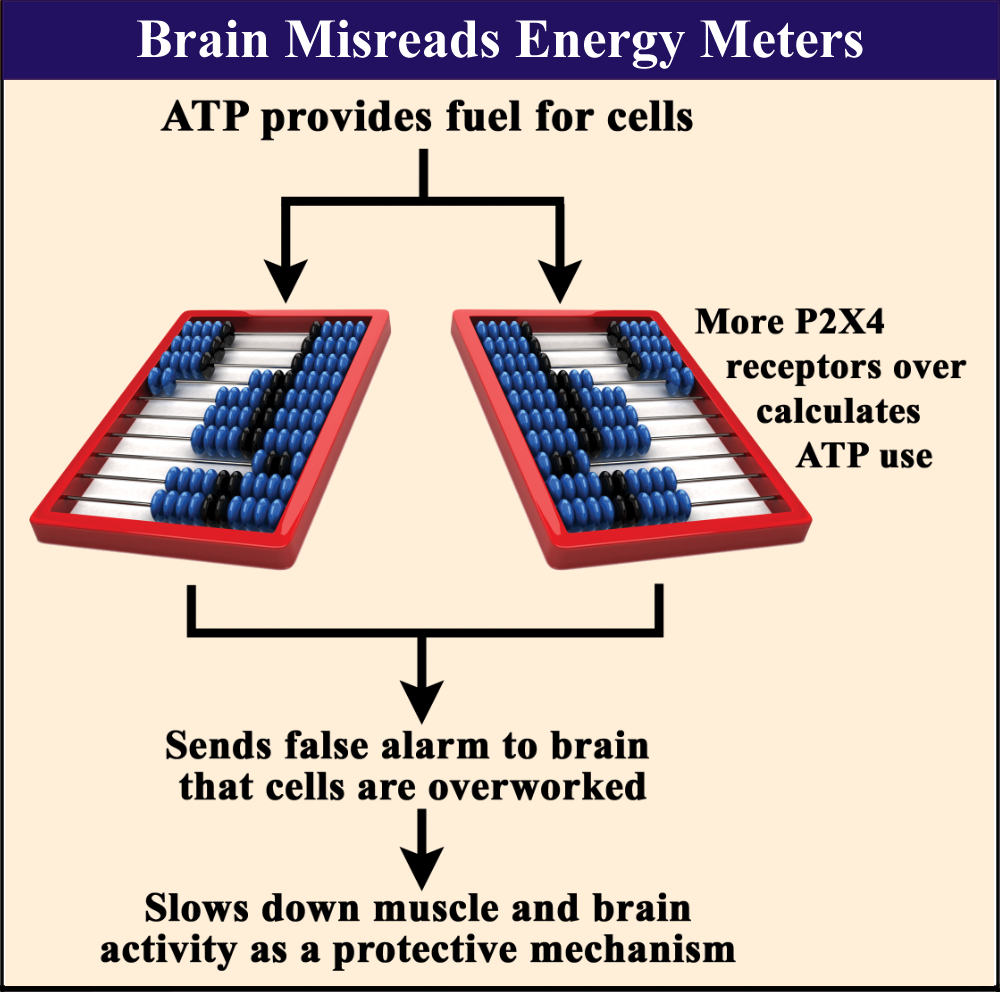
If you have too many P2X4 receptors, which looks to be the case for fibromyalgia patients, your muscle cells are getting double-billed for each molecule of ATP consumed. As a result, your brain may be falsely operating under the assumption that your muscle cells are working overtime. This could lead to amplified sensations of pain and fatigue, and abnormal blood flow to your muscles.
Keep in mind that your brain cells have an ATP abacus too that operates off of P2X-type receptors (some of which are of the P2X4 variety). Like the protective mechanism in your muscles to force cells to rest, your brain puts to sleep those cells with the highest daytime activity. Cells with the highest ATP use have the greatest propensity to fall asleep.
“You have two different phenomena,” says Light. ”One is brain fatigue and the other is genuine sleep. The fatigue is not really sleep, but it’s a sensation that pushes you toward sleep.”
Just like your muscles, your brain cells may be operating off false information from too many P2X-type receptors. Your brain may feel worn out, but unable to reach deep level sleep. This may occur when the running tab for the amount of ATP consumed by your brain cells is inaccurate. As a result, you end up in a quasi-sleep state day and night.
Pain Sensors
TRPV1 receptors are located on your nerve endings and immune cells to sense chemicals that could lead to cell injury and a painful state. For example, the TRPV1 receptors are well-known for detecting burning pain when chili peppers are applied to the skin. Hot peppers contain capsaicin, a chemical that is a potent activator of TRPV1 receptors. Elevated levels of acids, reactive/inflammatory substances, ATP, heat, and other agents can stimulate the TRPV1 receptor.3
In a resting state, Light found fibromyalgia patients had a much higher than normal demand for making TRPV1 receptors (based on genetic information from the blood leukocytes). According to Light, “Elevated TRPV1 receptors say fibromyalgia patients should be super sensitive to the production of pain-promoting metabolites.”
The heat-sensing abilities of TRPV1 receptors can offer interesting clues as to why your body functions the way it does. “As you exercise your muscles, they generate heat and other metabolites that activate the TRPV1 receptors,” says Light. With a higher number of receptors, the following symptoms may occur:
- After just a few minutes of exercise, your muscles sound off the pain alarms.
- If you exercise in short spurts throughout the day on a regular basis, this may do more than help you stay fit. The repeat bursts of heat in the muscles can work like capsaicin to reduce your number of TRPV1 receptors and lead to less pain.
- If you stop your exercise program for a few days, be prepared to start at square one because your TRPV1 receptors will be back in full force.
- Feeling cold all the time? Light says this could be the result of too many TRPV1 receptors. Core body temperature can be decreased and this may possibly tilt the scales to promote increased weight gain.
- Daily warm baths make you feel better because the regular heat can force your body to make less TRPV1 receptors.
Light suspects that TRPV1 and P2X4 receptors, along with others, work as a complex unit to regulate cellular functions and keep your brain informed. When you have a cold or other infection, both receptors can be further “revved up” according to Light, and this could greatly intensify your symptoms. So, get plenty or rest and take hot baths when recovering from your symptoms.
Sleep Disruption
Elevated IL-10 occurs in patients with severe insomnia and is believed to be a marker for disturbed sleep.4 People who sleep soundly throughout the night do not have increased production of IL-10. Whether IL-10 is the cause or the result of disrupted sleep is still being debated. Either way, the increased levels of IL-10 in people with fibromyalgia means that you are not sleeping well at night.
Abnormal production of the TRPV1 receptor could also be contributing to your poor sleep. This receptor is strongly tied to your body’s temperature regulation system, which in turn, plays a role in controlling your sleep-wake cycle. It’s all part of your internal clock that signals the timing of various processes (such as sleep) and hormonal secretions. No single element controls everything. Just as the violin contributes to the sound of an orchestra, body temperature plays a role in sleep.
Too many TRPV1 receptors mess with your thermostat control. After all, this receptor is activated by heat. “It not only contributes to pain, but also disrupts sleep,” says Light. “It may be responsible for the common patient perception of being ‘cold’ all the time. The TRPV1 receptor plays a role in the body’s thermal set-point.”
The Next Step
Light’s finding of three baseline biomarkers for fibromyalgia is a major milestone. Not only does it represent the beginning of an objective blood test, the three markers identified so far provide a logical basis for the symptoms and functional limitations of people with fibromyalgia.
After this AFSA-funded project appeared in the medical journals, Light used the data to receive an NIH grant. In addition, several other investigative teams have confirmed elevations in IL-10. This immune cytokine substance is known for its role in reducing inflammation. Recently, an AFSA-funded project confirmed low level inflammation in the brains of people with fibromyalgia. In addition, other research studies have also shown low levels of systemic inflammation.
- Light AR, et al. J Intern Med 271(1):64-81, 2012. Free Journal Report
- Light AR, et al. J Neurophysiol 100:1184-201, 2008. Free Journal Report
- Schumacher MA, Pain Pract 10(3):185-200, 2010. Free Journal Report
- Wang MF. Pediatr Neonatal 50(5):222-29, 2009. Free Journal Report
