Possible Causes
Autonomic Dysfunction
Your brain and spinal cord are supposed to communicate with other control systems in the body so that everything functions smoothly. But when the central nervous system (CNS) is busy handling the barrage of noxious signals from the cord, it can’t smoothly coordinate the function of your other organ systems.
Communications between your CNS and all your peripheral organs are transmitted through your autonomic nervous system. Naturally, a key organ is your heart (as shown in the diagram below), but all your organs are controlled by your autonomic system.
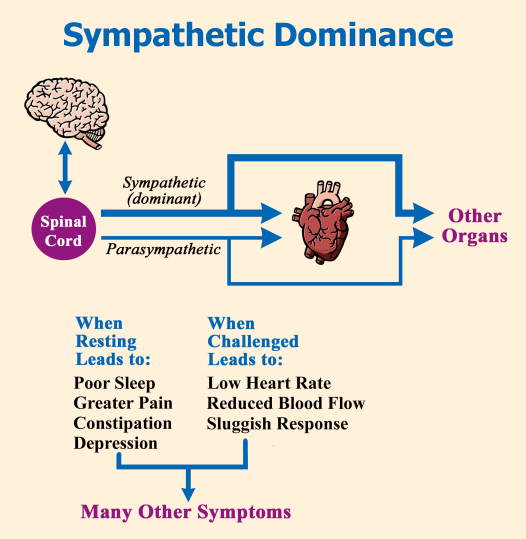
The autonomic system uses two opposing controllers: your sympathetic branch and your parasympathetic branch. The sympathetic branch is often called your “fight or flight” system, while your parasympathetic branch is one that enables “restfulness and digestion of food.” Ideally, your sympathetic system should be more dominant during the daytime to enhance alertness, while your parasympathetic should be the dominant system at night to promote sleep.
For your autonomic system to effectively respond to the demands of your body, it needs to operate with a lot of wiggle room. In particular, the control dial for your sympathetic system should be able to zoom from zero to ten in a split second to respond to the unpredictability of your environment. Both branches must be highly adaptive to change, such as dealing with an injury, infection, or emergency (dashing out of a burning building).
When your parasympathetic branch is overpowered by your sympathetic controls, many symptoms may surface (or if already present, they can become aggravated). You may find it hard to relax and your muscles may feel tense all the time. Digestion can be sluggish, contributing to abdominal bloating and cramping. Your sleep is so light that you seem partially awake and aware of your surroundings all night long. The deeper stages of sleep may be less likely to occur. Eyes and mouth can become excessively dry.
In fibromyalgia patients, the sympathetic dominance can lead to (or contribute to) the following symptoms:
- Low heart rate during exercise
- Reduced blood flow to the muscles, causing cold extremities and making exercise difficult
- Painful knots in the muscles, contributing to the development of myofascial trigger points or MTPs, which in turn generate electrical signals that ramp up the CNS
- Orthostatic intolerance or light-headedness because not enough blood pumps to the brain when going from sitting to standing
- Reduced saliva and tear production, causing dry eyes with vision problems and dry mouth (50 percent drop in saliva production during exercise has been reported)
- Disrupted sleep (the parasympathetic system is supposed to take over during the night but it doesn’t)
- Slowed digestion (irritable bowel, constipation, and acid reflux because stomach is slow to empty)
- Irritable bladder
- Burning skin
- Abnormal sweating
An abnormal functioning CNS is bound to spill over into a dysfunctional autonomic system. But the problem goes deeper than this. When your peripheral organs do not operate properly, they can send distress signals into your CNS and this can lead to a viscous cycle. So, how do you help restore some balance to your autonomic system so that your symptoms do not spiral out of control? The key is to do everything you can to increase the activation of your parasympathetic system.
Relaxing warm baths help enlist the parasympathetic branch, and if done before bedtime, it helps with sleep. Better quality sleep helps push back on the sympathetic dominance. Anything you can do to help restore your autonomic system balance will also reduce the strangle-hold that your sympathetic branch has on restricting muscle blood flow. Again, heat helps along with gentle movement (perhaps coupled with relaxation breathing).
Another approach is to reduce your number of myofascial trigger points (MTPs) because they send a constant barrage of signals into your CNS. In turn, these inputs get amplified by the CNS and then they are distributed throughout your muscles to make them hurt and set up more MTPs. See the section on Muscle Pain Relief for help.
What about medications for treating an overactive sympathetic system? It’s possible that a small dose of a beta-blocker, such as propranolol might help. The downside of this drug is that it reduces blood pressure and there are no placebo-controlled trials to prove its efficacy. On the flip side, you should probably steer clear of medications that jack up the sympathetic system, such as nasal decongestants containing pseudoephedrine (a cousin of epinephrine).
