Fibromyalgia Basics
What’s Driving Your Pain?

The 18 tender points that were used to diagnose fibromyalgia are more than just sore areas on the body of patients. Ninety percent are myofascial trigger points (MTPs), according to an AFSA-funded study by Hong-You Ge, M.D., Ph.D., of Aalborg University in Denmark.1 More importantly, these trigger points make your fibromyalgia pain worse.
Importance of MTPs
Why is Ge’s finding so important and what does it matter if the painful areas on your body are called tender points or myofascial trigger points? Identifying tender points required a patient’s feedback during an exam, making them a subjective finding. Besides, tender points were never viewed as a physiological abnormality that could be treated. On the other hand, MTPs are an objective finding, they contain pain-sensitizing chemicals, and there are methods to treat them.2
MTPs are hard nodules in tight, ropy muscle bands that shorten the muscle and restrict movement. These nodules exist because the muscle fibers in the area are contracted. However, the ability of a healthcare provider to locate your MTPs depends upon their skill level. Fortunately, Ge used intramuscular electromyography (EMG) to objectively identify the MTPs in the fibromyalgia patients used in his study.
EMG involves inserting a small, thin needle into the MTP (located first by palpation). MTPs generate a substantial amount of electrical activity, and the EMG needle picks up this signal. As a result, the MTP location is confirmed and doesn’t rest on the skill of the examiner or patient feedback. However, you may wonder: why do trigger points generate electrical activity in resting muscles?
MTPs consume energy to maintain their tightly contracted and knotted state. In the process, they also give off a continuous stream of electrical signals. Yet, inserting the needle into the heart of the MTP forces it to release the contraction and the electrical signal on the EMG drops to nothing. In fact, this is the same mechanism used by a technique called dry needling to relieve MTPs. Except when dry needling, a tiny acupuncture needle is inserted to release the MTP and force the muscle to relax.
Two Types of MTPs
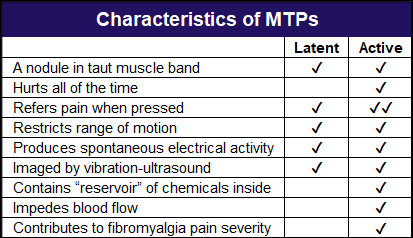
There are two types of MTPs: active and inactive (latent). Active MTPs hurt all the time. You don’t have to press on them or move the muscle they reside in to know they exist. The active forms are the focus of treatment. Although latent MTPs restrict range and hurt when pressed, they are not the serious troublemakers. Keep in mind, however, that overusing muscles can easily convert your latents into active MTPs.
Ge assessed the discomfort generated by the MTPs at the predefined tender point sites. These areas produced most, but not all the pain felt by the fibromyalgia patients in the study. So, other sites with active MTPs contribute to your pain. Ge found a high incidence of active MTPs in the mid-back region and the upper arms.
The diagram below shows the areas where Ge found the most common MTPs in fibromyalgia patients. The black dot areas coincide with 18 tender points, while the two red dots were also found in patients. In fact, the low back MTP was the most prevalent, and it was not included in the initial diagnostic exam of fibromyalgia patients.
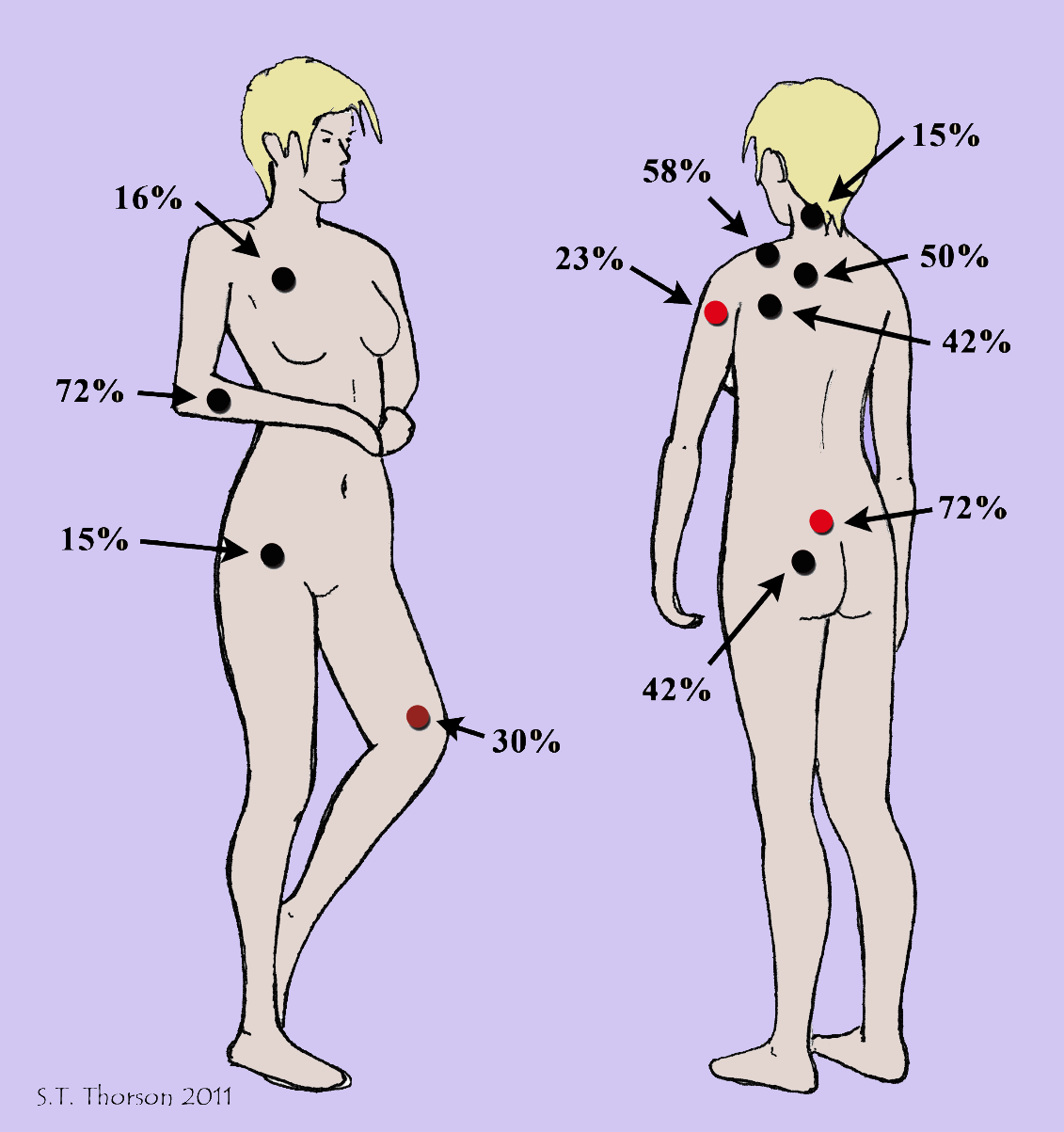
Ge identified an important relationship between MTPs and overall pain severity. The greater the number of active MTPs, the worse the fibromyalgia patient’s pain. On the other hand, the number of latent MTPs did not affect each patient’s pain rating.
Why do active MTPs impact your pain, while latents don’t influence it? Active MTPs are much more evolved and contain a buildup of nasty chemicals (like a “reservoir”). These substances can irritate nerve endings and help explain why active MTPs produce pain, even when you are not moving.3 Blood flow through the active (but not latent) MTPs is also impeded.
MTPs & Your Nervous System
MTPs are not just areas in the muscle where the fibers are contracted, and the chemicals are shored up. They are also generators of electrical activity. The electrical signals produced by MTPs are transmitted to the central nervous system and can keep it “fired up.” So, not only do active MTPs hurt, but they also rev up the central nervous system. In turn, your central nervous system sends amplified signals to muscle groups in other body regions to spread your discomfort.
Ge’s study shows that the muscle tissues are important contributors to the pain of fibromyalgia. Active MTPs may possibly be a source of electrical input that maintains your dysfunctional central nervous system state. And once this happens, the nervous system sends out signals to the muscles to potentially cause more MTPs to form.
Muscle Cramps & Weakness
If you suspect fibromyalgia makes you more prone to muscle cramps, you are correct. The mere presence of pain in a muscle increases the odds it will cramp.4 The widespread pain of fibromyalgia lowers the cramping threshold, especially in muscles containing active MTPs. In fact, if knifelike leg cramps are destroying your sleep, try the following:
- Gently stretch your leg and foot muscles in warm water before bedtime.
- Take a calcium and magnesium supplement in the evening.
- If a Charlie horse occurs, pull your heel in the direction of the cramped muscle. This technique further shortens the fibers so they can relax.
Muscles with MTPs wear out faster than normal and this promotes the development of more MTPs in neighboring muscles.5 Naturally, repetitive use or overloading a muscle will intensify your sense of muscle weakness. Unfortunately, fatigue in fibromyalgia is complicated. While you feel as though your muscles have no power, a large part of this sensation is caused by your central nervous system controls.
Patient Recommendations
“Active MTPs are important pain generators in fibromyalgia,” says Ge. “Targeting active trigger points should significantly relieve fibromyalgia pain and represents a promising treatment potential.”
Although 90 percent of the predetermined 18 tender point sites were found to contain MTPs, not all of them were of the “active” variety. Muscles in the back shoulders, buttocks, and upper forearm regions were most likely to contain active MTPs, but this is only based on the 18 tender point sites. “Examining physicians should check active MTPs in all muscles according to a patient’s pain drawing,” says Ge.

Trigger points are structural abnormalities in your muscles and there are many ways to treat them. One possible approach is dry needling by a highly skilled practitioner, usually a physical therapist. “Relief of active MTPs will decrease fibromyalgia pain intensity and significantly reduce the input that maintains the dysfunctional nervous system,” says Ge.
“Before long-term pain relief is obtained, perpetuating factors for the development and maintenance of MTPs must be resolved,” says Ge. “In this respect, acute and chronic muscle overload can easily cause pain reoccurrence. MTP therapy should be continued at some regular interval (once a week, once a month, etc.) tailored to each patient. If pain in one body region returns, this is a good indicator for seeking immediate treatment.”
In addition to getting professional help with deactivating your MTPs, have a daily home program to reduce muscle tightness and pain. Submerging your body in soothing warm water (or applying a moist hot wrap) relaxes muscles and improves circulation. Even if you cannot afford a massage therapist, an electric massager with a long handle can offer relief. The goal is to keep your muscles as healthy and functional as possible.
Start with Your Trapezius
If active MTPs in multiple muscles are the driving force for your widespread fibromyalgia pain, where should treatment be focused? One possibility is your trapezius, the large shoulder muscle located in your upper back region. It’s a troublesome area that most all fibromyalgia patients state is painful.
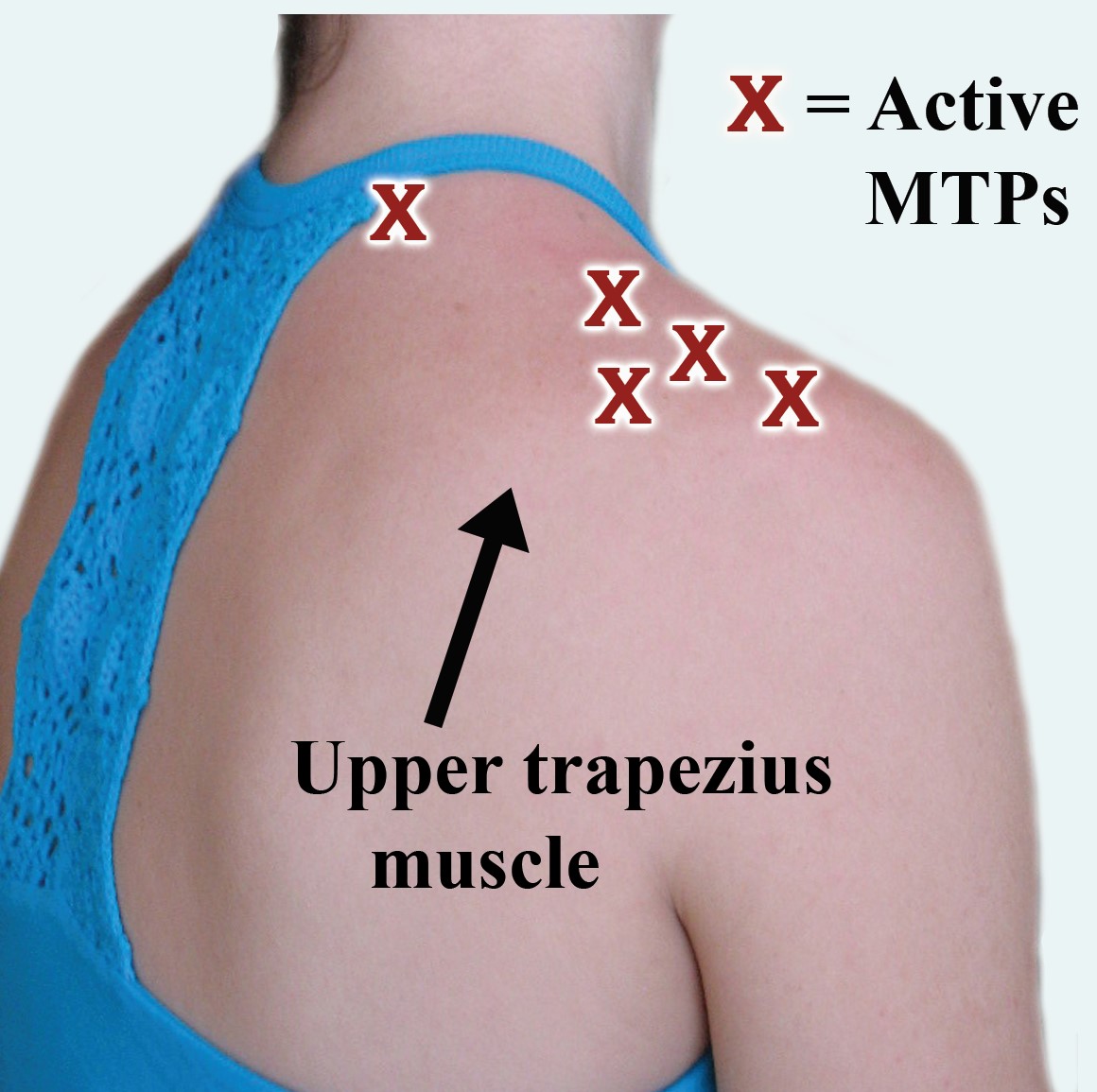
Ge sought to determine how many MTPs might be present in the two trapezius muscles as another part of his AFSA-funded study.6 He used needle EMG to map out active and latent MTPs in fibromyalgia patients and healthy subjects.
The average fibromyalgia patient had almost five active MTPs and four latents on each side of the trapezius muscle. The healthy subjects did not have any active but had five latent MTPs in the same muscle region. The pain pattern produced by the MTPs (active and latent) in fibromyalgia patients covered the head, neck, shoulders, mid and lower back, upper chest, and arms. In other words, your trapezius muscles are contributing to the brunt of your upper body pain.
Bottom line: Treating the MTPs in your upper trapezius muscle is a good place to start. Also, avoid over straining your shoulder muscles because they are already overloaded with MTPs (minimize leaning your head forward).
Stay Current on Treatments & Research News. Sign up for a FREE membership today!
Read more about myofascial trigger points (MTPs) in our section on Muscle Pain Relief or learn about other Symptoms. For different approaches to target your fibromyalgia, see our sections on Medications, Alternative Therapies, and Diet & Nutrition.
References for What Makes Fibro Worse
- Ge HY, et al. J Pain 11(7):644-651, 2010. AFSA-funded Study Article
- Pradeep A, et al. BMC Musculoskelet Disord 24(1):624, 2023. Free Article
- Shah JP, et al. PM & R 7(7):746-761, 2015. Free Article
- Serrao M, et al. Exp Brain Res 187:623-629, 2007. Abstract
- Ge HY, et al. Pain Med 13:957-64, 2012. Free Article
- Ge HY, et al. PAIN 147(1-3):233-40, 2009. AFSA-funded Study Abstract
