Possible Causes
Gut Influences in Fibromyalgia
One’s cognitive functions, emotions, state of mind, and overall health (including the presence of chronic pain) are influenced by the bugs living in the gut. Digestive tract microbes (called your microbiota) form a diversified ecosystem. It’s a living community capable of altering the way your central nervous system (CNS) functions … and so much more. In fact, research shows that gut microbes influence fibromyalgia symptoms.
Your microbiota is ten times greater than the number of cells residing outside your digestive system. Just based on size alone, John F. Cryan, Ph.D., of the University College Cork in Ireland, says, “The gut microbiota are often referred to as the forgotten organ.”1 Fortunately, microbiota research is a hot topic in fibromyalgia and recent findings offer tremendous hope for patients.
Beyond Digestion …
Many fibromyalgia treatments focus on medications that raise serotonin levels in the CNS. Serotonin works as a pain-fighting and mood-enhancing chemical, but most of it is made in the gut, not the CNS.2 When you ingest foods containing tryptophan (an amino acid building block of protein), your microbiota convert it into serotonin.
Serotonin is not the only pain-fighting chemical that is influenced by your microbiota. When you ingest glutamate (another amino acid building block of protein), your gut microbes can convert it into GABA. Although glutamate works in your CNS to cause pain, GABA does the opposite – it relieves pain. In addition, GABA calms you down and reduces anxiety. If you don’t have enough microbes to convert glutamate into GABA, this will cause more pain and anxiety.
Other pain-relievers (such as dopamine) and hormones (such as cortisol) are also influenced by your microbiota. In addition, various vitamins (such as vitamin K) can only be manufactured by your gut microbes. Even your bile acids (produced by your liver to help with fat digestion) are transformed by your gut microbiota to cause painful symptoms. Certain microbes turn the bile into analgesic substances while others transform it into pain-enhancing chemicals.
The point is, the bacteria inhabiting your gut do much more than digest your foods. And when it comes to chronic, painful diseases like fibromyalgia, your microbiota can influence your symptoms.
Intricate Network
The gastrointestinal (GI) tract is surrounded by a massive network of neurons that is as intricate as your spinal cord. These GI neurons form a two-way communication highway with the CNS.
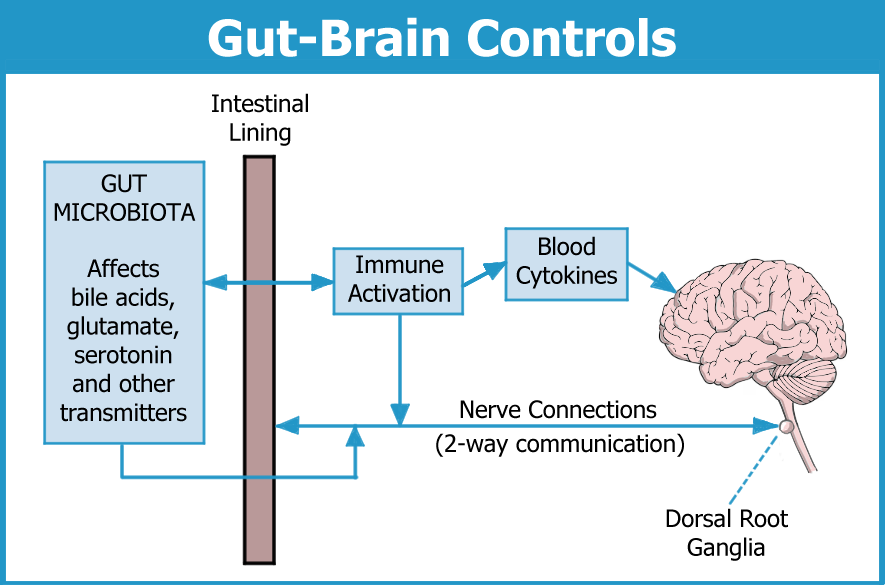
The neurons surrounding the GI tract are not the only way your microbiota can influence your CNS. More than 70 percent of the body’s immune cells reside alongside the digestive system. These cells are influenced by the types of microbes growing in your gut, even if they aren’t dangerous pathogens. This is another way of alerting your spinal cord and brain about potential problems in the GI system.
Any undesirable changes in your microbiota will prompt your immune cells to pump substances into the bloodstream. Cytokines are one of the more common signaling chemicals released by immune cells. They can enhance pain, cause depression-like symptoms, and interfere with cognitive functions. Cytokines can enter the CNS and activate immune cells called the microglia. Once activated, the microglia can disrupt brain functions, leading to pain, fatigue and other symptoms.
Aside from the brain, other structures that appear to be under attack by the immune system are the dorsal root ganglia. These are tiny little bulb-shaped structures up and down the entrance to the spinal cord. They are surrounded by satellite glial cells – immune cells like the microglia. Whether gut microbes play a role in this attack remains to be determined. For more details, see our article: Is Fibro an Autoimmune Disease?
Microbiota Changes
Research shows that fibromyalgia patients possess undesirable alterations in their gut microbiota that are contributing to the condition and possibly causing it.3 A study headed up by Amir Minerbi, M.D., Ph.D., of Israel, shows an imbalance of 19 microbial species in fibromyalgia patients compared to healthy controls. Some are much more abundant while others are nearly depleted, but how do these changes relate to symptoms?
The degree of microbiota alterations corresponds to greater pain intensity, worse fibrofog, and more fatigue. Based on the differences in the microbiota, Minerbi’s team distinguished fibromyalgia patients from healthy controls 88 percent of the time. Although microbiota analyses are too expensive to use for clinical practice, the technology is changing. It’s possible that this test could be affordable down the road.
“The ability of our model to accurately identify fibromyalgia patients in this study indicates that the gut microbiota may have the potential to contribute to the diagnosis,” says Minerbi.
Three key findings by Minerbi to help you appreciate why your gut could be at the root of your fibromyalgia are:
- Species that fight inflammation to reduce immune activation and cytokine production are depleted. These same bacteria play an important role in protecting the gut lining, which prevents bacterial products from entering the bloodstream.
- Microbes that transform bile acids into pain-sensitizing substances are increased.
- Most of the abnormalities found in the fibromyalgia group are also documented in the related condition of chronic fatigue syndrome (CFS/ME). So, if you have this diagnosis due to substantial fatigue, the overlap is substantial.
Alterations in the microbiota can trigger immune system alarms and the release of cytokines into the blood. And if the gut lining becomes “leaky,” bacterial products in the blood will sound off more distress signals within the immune system. Many studies already show increased levels of blood cytokines in fibromyalgia patients, and it’s possible they originate from the cells lining the gut. In addition, the glial cells at the entrance to the spinal cord might also be the target of an immune attack.
Bile Acids
As mentioned above, gut microbes that convert bile acids into nerve-irritating substances endings are increased. In another study by Minerbi’s team, microbes that change bile acids into analgesic agents are one-fifth that of normal.4 The net result is that bile acids in fibromyalgia patients are ramping up pain. In fact, this imbalance in bile-transforming bacteria correlates with the symptoms of pain, fatigue, fibrofog, and unrefreshing sleep.
Altered bile production is thought to lead to increases in blood products that activate the dorsal root ganglia. In turn, activation of these structures can boost the intensity of the signal before it enters the spinal cord. A stronger signal means more pain, and it can spill over into other symptoms associated with fibromyalgia. Changes in bile may also alter the way your body processes fats. Quite possibly, this may explain why fibromyalgia patients have excessive deposits of fat in their blood and muscles. See Altered Metabolism for more details.
Glutamate
Another research team in Spain, headed up by Felix Royo, Ph.D., confirms that fibromyalgia patients have an altered microbiota.5 In particular, two species of bacteria that convert glutamate into GABA are depleted. Remember, glutamate enhances pain while GABA relieves it. On the other hand, Royo found elevations in bacteria that produce glutamate and similar pain-promoting transmitters.
Increases in gut microbes that produce glutamate is one thing, but can it lead to increases in this pain transmitter in the blood? It turns out, the answer is “yes.” Royo found significantly elevated blood glutamate levels in the fibromyalgia patients compared to controls. He suspects glutamate enters the bloodstream due to leakage in the intestinal lining. Then the transmitter activates the neurons surrounding the gut to signal the brain and spinal cord, leading to more pain.
What Can You Do?

If gut microbiota imbalances are the source of your symptoms, what can be done to counter them? Studies show that the diet of people with fibromyalgia is the same as that of healthy, pain-free control subjects.6 So, abnormal eating habits probably are not causing the gut dysfunction. Yet, there are a few foods thought to reduce bile acids: avocados, blueberries, and walnuts.
The ideal diet for a healthy gut consists of fresh fruit and vegetables, low fat meat, and high fiber foods. Refined sugar, vegetable oils, and refined cereals should be avoided as much as possible. Whether such a diet will help is unknown, but it can’t hurt. Also, try to reduce dietary glutamate (such as MSG and other flavor enhancers). Bacteria needed to convert glutamate into GABA are deficient in fibromyalgia, which may be why the diet helps. See the Diet & Nutrition section for guidance on eliminating glutamate.
Due to the complexity of the microbiota, it’s nearly impossible to produce an impact with any of the probiotics currently on the market. None of them specifically target any disease.
Microbiota-based therapeutics are the wave of the future. It consists of specially formulated capsules full of microbes and the FDA is already on board with this technology. Instead of prescription drugs, fibromyalgia patients may eventually be prescribed capsules to favorably alter the gut microbiota.
New Research
Still uncertain about the role the gut plays in producing your fibromyalgia symptoms? A recent multi-center study provides compelling evidence. Transfer of gut microbiota from fibromyalgia patients to mice causes a rapid onset of pain in the mice. It even produces many of the CNS changes that are found in people with fibromyalgia, such as microglia activation.7 In addition, transfer of gut microbiota from healthy subjects into fibromyalgia patients significantly reduces symptoms.
Stay Current on Treatments & Research News: Sign up for a Free Membership today!
Medications | Alternative Treatments | Fibro Friendly Exercises | Research News | Why So Many Symptoms
Back to Peripheral Systems; Next to Hyped-Up Ganglia
References for Gut Microbes & Fibromyalgia
- Cryan JF, Dinan TG. Nat Rev Neurosci 13(10):701-12, 2012. Abstract
- Roth W, at al. Int J Mol Sci 22:2973, 2021. Free Report
- Minerbi A, et al. PAIN 160(11):2589-2602, 2019. Abstract
- Minerbi A, et al. PAIN 164(2):e66-e76, 2023. Abstract
- Clos-Garcia M, Royo F, et al. EBioMedicine 46:499-511, 2019. Free Report
- Minerbi A, at al. Int J Environ Res Public Health 19(6):3254, 2022. Free Report
- Cai W, Shir Y, Minerbi A, Khoutorsky A, et al. BioRxiv October 28, 2023. Free Report
